Brain imaging reveals dynamic changes caused by pain medicines
A study in the December issue of Anesthesiology suggests a role for brain imaging in the assessment and potential treatment of chronic pain.
University of Michigan researchers are the first to use brain imaging procedures to track the clinical action of pregabalin, a drug known by the brand name Lyrica® that is prescribed to patients suffering from fibromyalgia and neuropathic pain.
Three different brain imaging procedures were performed – proton magnetic resonance spectroscopy, functional magnetic resonance imaging and functional connectivity magnetic resonance imaging – in 17 patients with fibromyalgia.
Fibromyalgia is a chronic pain disorder thought to result from a disturbance in the way the central nervous system processes pain. It affects an estimated 10 million people in the United States and 3 to 6 percent of the world population.
Patients with fibromyalgia may spontaneously report pain throughout their bodies although there is no inflammatory or anatomical damage. In addition to chronic pain, patients may also suffer from related mood disturbances, such as anxiety and depression.
Previous research has shown that fibromyalgia patients may have heightened neural activity in a region of the brain involved in processing pain and emotion called the insula, and that this excess activity may be related to elevated levels of the excitatory neurotransmitter glutamate.
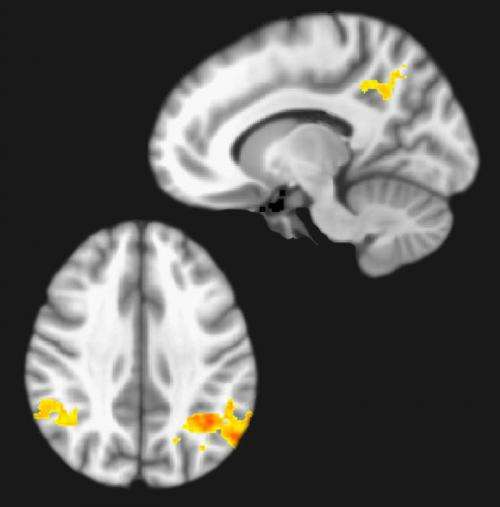
Brain imaging conducted at the U-M Health System suggests pregabalin works in part by reducing the concentration of glutamate within the insula, which is consistent with animal studies. These reductions in glutamate were also accompanied by decreases in insula connectivity and reductions in clinical pain ratings.
This type of brain activity imaging may help in the development of new pain medicines and personalized chronic pain treatment.
"The significance of this study is that it demonstrates that pharmacologic therapies for chronic pain can be studied with brain imaging," says lead study author Richard Harris, Ph.D., assistant professor of anesthesiology at the University of Michigan.
"The results could point to a future in which more targeted brain imaging approaches can be used during pharmacological treatment of chronic widespread pain, rather than the current trial-and-error approach."
More information: "Pregabalin rectifies aberrant brain chemistry, connectivity and functional response in chronic pain patients," Vol. 119, Issue 6, December 2013, Anesthesiology, the Journal of the American Society of Anesthesiologists.

















