Common blood cancer may be initiated by single mutation in bone cells
Acute myeloid leukemia (AML) is a blood cancer, but for many patients the cancer may originate from an unusual source: a mutation in their bone cells.
In a study published today in the online edition of Nature, researchers at Columbia University Medical Center (CUMC) found that a mutation in the bone cells called osteoblasts, which build new bone, causes AML in mice. The mutation was found in nearly 40 percent of patients with AML or myelodysplastic syndrome (MDS), a precursor condition, who were examined as part of the study.
The researchers were able to stop production of leukemic blood cells in the mice with a drug that blocked the effects of the osteoblast mutation, suggesting that a similar drug may benefit a large portion of AML and MDS patients.
"If the mutation works the same way in humans, our study suggests practical ways that we may be able to intervene with a drug or an antibody. It may give us a tool for a disease that is rarely curable," said the study's lead investigator Stavroula Kousteni, PhD, associate professor of medical sciences in medicine and physiology & cellular biophysics at CUMC.
"This paper goes to the heart of bi-directional translational research, as it represents collaboration between institutions, as well as between clinicians and basic scientists," said Azra Raza, MD, director of CUMC's MDS Center and a co-author of the study. "The Kousteni Lab made the observation that a mutation affecting b-catenin in the bone marrow microenvironment cells of mice can cause leukemia. Clinicians from Memorial Sloan-Kettering and CUMC then extracted bone marrow samples of patients with MDS and AML from their tissue repositories, to confirm a similar pathway in a subset of patients. This incredibly important observation opens the possibilities of novel therapies for these dreaded diseases using non-chemotherapeutic approaches."
AML is one of the most common types of leukemia in adults, with about 15,000 cases diagnosed in the U.S. each year. The disease progresses rapidly, and only about 25 percent survive three years after diagnosis. MDS is a group of blood disorders diagnosed in about 10,000 people in the U.S. each year. Many people with MDS eventually develop AML.
Mutation of beta-catenin gene in osteoblasts causes AML in mice
In the current study, Dr. Kousteni and colleagues investigated a mouse strain that dies soon after birth from severe blood abnormalities. They found that the disease, which was the same as AML, was caused by a mutation in the beta-catenin gene in the animals' osteoblasts.
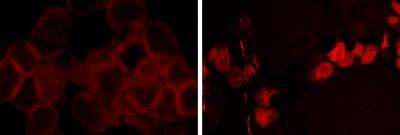
The mutation leads to cancer in adjacent bone-marrow stem cells through a series of events. First, the mutated beta-catenin protein moves from its normal location on the exterior of the osteoblast to the cell's nucleus, where it turns on production of a protein called jagged1.
Jagged1 proteins are then shipped to the osteoblast's exterior membrane, where they can bind to Notch proteins—which activate signaling pathways—on neighboring bone-marrow stem cells. When this happens, Notch transmits signals inside the bone-marrow stem cells that ultimately transform the cells to leukemia.
When they looked at cells from AML and MDS patients, the researchers documented similar changes in beta-catenin, jagged1, and Notch signaling in 38 percent of the patients.
"Previous studies have shown that osteoblasts and leukemia blasts communicate with each other," said Ellin Berman, MD, a co-author of the study and leukemia clinician at Memorial Sloan-Kettering Cancer Center. "This study is the first to clarify exactly how that may happen."
New concept in cancer treatment
This study is the first to show that a mutation in one cell not only can influence nearby cancer cells but can cause cancer in another type of cell. Treating cancer by targeting nearby cells is a novel concept in cancer treatment, says Dr. Kousteni. "You're treating a cancer by targeting a cell that doesn't change— instead of chasing the cancer cells, which constantly mutate and change.
"In AML, targeting jagged1 may stop the creation of new malignant cells; it would likely be used in combination with cytotoxic therapy. The first drug would prevent the emergence of new malignant cells; the second would eradicate the existing ones.
"The findings in this paper have crucial implications for our patients," said Siddhartha Mukherjee, MD, PhD, assistant professor of medicine at Columbia and a co-author of the study. "We have a growing armamentarium of drugs that target and kill cancer cells. But if cancer arises because of an interaction between a cell and its environment, we could potentially target that environment as well. Indeed, the cancer 'microenvironment' might be more amenable to drug therapy, as it likely has less of a propensity to mutate. At Columbia's MDS Center, we have been banking tissue samples of this cancer microenvironment, in addition to cancer cells. We hope to unleash all the resources now deployed on cancer cells to learn about, and target, cancer microenvironments,- the 'homes' that cancers grow in."
More information: The paper is titled "Leukaemogenesis induced by an activating β-catenin mutation in osteoblasts."















