Bacteria in the lungs make COPD patients sicker
(Medical Xpress)—Conventional wisdom has held that even though bacteria persist in the lungs of patients with chronic, obstructive pulmonary disease (COPD), their presence, referred to as 'colonization,' is innocuous so long as the patient isn't having a flare-up, or exacerbation, of respiratory symptoms.
Now, a new study by researchers at the University at Buffalo School of Medicine and Biomedical Sciences in cooperation with the U.S. Department of Veterans Affairs shows that COPD patients do experience more respiratory symptoms when their lungs are 'colonized' by bacteria, even in the absence of an acute exacerbation.
The paper was published online last month as an article in press in the Annals of the American Thoracic Society.
COPD, which is most commonly caused by smoking and includes chronic bronchitis and emphysema, compromises the lungs' innate defense against bacteria, allowing bacteria to persist.
In previous work, these UB researchers illustrated that having bacteria in the lungs in COPD is associated with increased inflammation. This study takes the next step by proving that such bacterial colonization is sufficient to trigger clinically significant increases in shortness of breath, cough and sputum in COPD patients.
Several unique features of this study helped the investigators make this important observation: It is the first longitudinal study of symptoms in COPD during bacterial colonization with a well-validated tool for assessing symptoms; it also controlled for variables, such as local air pollution levels and weather-related factors, such as humidity, which can affect daily symptoms in these patients.
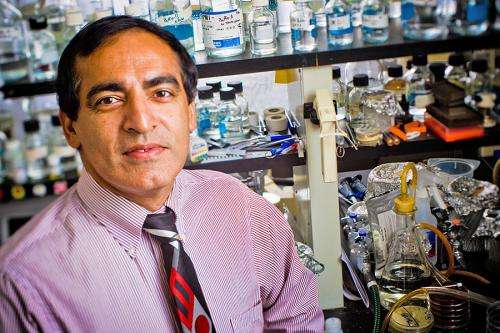
"These findings demonstrate that it's time for a paradigm shift in how we treat patients with stable COPD," says Sanjay Sethi, MD, senior author, UB professor of medicine and division chief of pulmonary, critical care and sleep medicine, director of the COPD Study Clinic and staff physician at the Veterans Affairs Western New York Healthcare System (Buffalo VA).
"The lungs are constantly being exposed to microbes 'with every breath you take' as well as from aspiration of small amounts of secretions from the throat, especially during sleep," Sethi says. "If the persistence of these bacteria contributes to increased symptoms and inflammation in the lungs in stable COPD, we should regard this as a chronic infection, not innocuous colonization. For that reason, more must be done to reduce chronic infections in COPD."
However, because of the risk of development of resistance, he says, long term antibiotics are not the answer.
"Instead, we need to go beyond traditional approaches of bronchodilation and anti-inflammatory agents to reduce symptoms," Sethi says. "We need to put more emphasis on developing therapies that can decrease bacterial colonization in COPD."
According to Sethi, clinicians have known that most patients with stable COPD experience daily fluctuations in respiratory symptoms but why this is so is not well understood. Furthermore, he says, even though these fluctuations often qualify as exacerbations in terms of intensity and duration, only a third of them are reported.
"Bad days and unreported exacerbations are at least partially explained by bacteria causing inflammation in the lower airways in COPD," says Sethi. "The role of infection in COPD is not fully documented, and this finding helps add to our understanding of how it affects patients on a daily basis."
The study focused on four common pathogens encountered in COPD: Haemophilus influenzae, Moraxella catarrhalis, Streptococcus pneumoniae and Pseudomonas aeruginosa. The researchers used sensitive molecular detection methods, as well as conventional laboratory cultures, to detect these bacterial pathogens.
The longitudinal study was conducted from October 2005 to January 2009 with 41 elderly male veterans with smoking-related COPD in the COPD Study Clinic at the Buffalo VA.
Patients used electronic diaries to record daily symptoms of breathlessness, cough and sputum. They were seen in the clinic each month, in addition to whenever they had exacerbations, providing sputum and blood samples in addition to clinical information. Sputum samples also were obtained every two weeks in the patients' homes.
Sethi notes that research support from the Buffalo VA and participation of patients was absolutely critical. "We can model inflammation and other effects of smoking using animals but documenting respiratory symptoms can only be done with human subjects," he says. "We could not have done this study without the generous participation of our patients."















