How gut bacteria can be harnessed as novel therapies for disease
Millions of years of coevolution have inextricably linked you and your microbiome, whose chemical "factories" help keep you healthy by doing such things as synthesizing vitamins and digesting your food. Recently, Professor of Biology Sarkis Mazmanian's laboratory has uncovered the surprising roles they play in fending off certain diseases.
Q: What do you do?
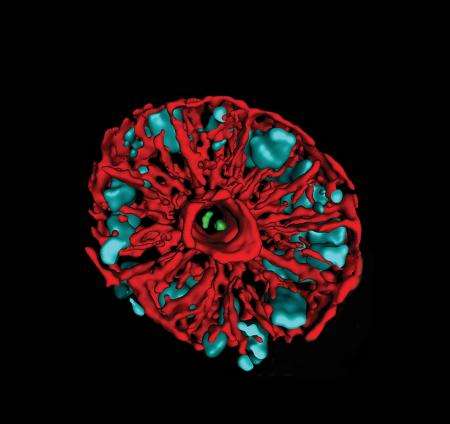
A: Our laboratory studies how beneficial microbes in the gastrointestinal tract interact with the immune and nervous systems. We each carry two to three pounds of bacteria—known as the human microbiome—in our bodies, and we have 10 times more microbial cells than we do human ones. We're outnumbered by an order of magnitude, but our cells are about 1,000 times bigger. Although most of these bacteria reside in our guts, in the colon, their metabolic products are found throughout the body. We think that these molecules can flip switches in biological circuits—even those in our brains. Pasteur knew about the bacteria in our intestines 150 years ago, but the evidence that some are beneficial is less than a decade old.
Q: As President Lyndon Johnson used to say, "How does this help Grandma?"
A: [laughs] As Sarkis says, "How does this change the world?" It's an entirely new perception. The game-changer is that we have found specific microbes that, at least in animal models, interact with the immune and nervous systems to ameliorate inflammatory bowel disease, multiple sclerosis, and even autism.
Western civilization has successfully controlled infectious, disease-causing microbes through antibiotics, vaccination, personal hygiene, and sanitation. These approaches are usually indiscriminate, and have also changed our association with microbes as a whole. And if some microbes are actively conferring health on us, say by secreting some substance that helps our immune system function properly, then removing them may result in disease.
We're all born sterile, and in the first three years of life we develop a complex consortium of microorganisms. Our first exposure is during the birthing process. Children born through natural childbirth are more resistant to allergies and autoimmune diseases than children who are born through C-sections, and the same is true with children who are breast-fed versus formula-fed. We don't yet know where the rest of our microbes come from, but my best guess is human contact. I mean, just think about human contact now, versus a thousand years ago. There's hand sanitizers, soap and water, indoor plumbing . . . We're not recolonizing ourselves, reexposing ourselves to our own microbes, let alone exposing our children to our adult microbes. Throughout human evolution there has been a cycle by which we have inoculated our kids, and I think we've disturbed—or even broken—that cycle.
We can now begin to think about supplementing or replacing those beneficial organisms, so I don't think it's far-fetched that, within a decade or so, doctors might examine your microbiome as well as looking at your lipid levels and your sugar levels and doing other routine diagnostics. And if they identify an organism that you are missing, you might be prescribed an FDA-approved pill that contains microbes—or microbial products—to restore the benefits you've lost.
Eating yogurt is not going to do it, nor will playing in the dirt, nor will the probiotics at health-food stores. None of those organisms coevolved with humans, so in essence they just pass through your system. This is a very important point: there's a distinction between the microbes in the environment and the microbes in your gut.
Q: How did you get into this line of work?
A: As a graduate student, I was studying Staphylococcus aureus, which causes staph infection. Staph infections are a huge problem in the community, and in hospitals, and we discovered some fruitful mechanisms to inhibit staph from causing disease. But as I was thinking about the next phase of my career, I read an article about all these bacteria that live in our gut that nobody was studying. And that interested me, so very, very quickly I decided that I was going to go into the unknown. I was just convinced, in this almost intuitive way, that all these bacteria must either be neutral, and were not doing anything—which is very unlikely, if you understand microbial metabolic processes—or that some subset of them must be doing something beneficial. Otherwise, why would they still be there? So I wanted to study the good guys, and I wanted to do what nobody else was doing. And this is the beauty of Caltech. We do the things here that nobody else is bold enough, or daring enough, to do.



















