Homes now 'reservoirs' for superbug MRSA
An antibiotic-resistant "superbug," long a problem in health-care settings, is now taking up residence in people's homes, a new U.S. study finds.
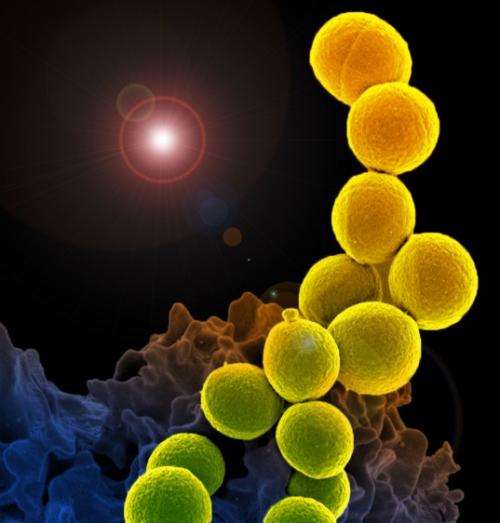
Methicillin-resistant Staphylococcus aureus, commonly referred to as MRSA, was once mainly confined to places like hospitals and nursing homes, where it can cause severe conditions such as pneumonia and bloodstream infections.
But since the late 1980s, MRSA has also hit the wider community, where it usually causes skin infections, some of them potentially life-threatening. The bug is spread by skin-to-skin contact or through sharing supplies such as towels or razors. And certain groups are at increased risk, including athletes in contact sports and people living in cramped quarters, such as military barracks or prisons.
But in the new study, researchers found that such communal spaces are not the only major MRSA "reservoirs" out there.
"What our findings show is it's also endemic in households," said lead researcher Dr. Anne-Catrin Uhlemann, of Columbia University Medical Center in New York City.
MRSA is called a superbug because it is resistant to many common antibiotics. The new results, published April 21 in Proceedings of the National Academy of Sciences, are based on 161 New York City residents who contracted MRSA infections between 2009 and 2011.
Uhlemann's team analyzed the genetic makeup of MRSA samples from those patients, and took swabs from a comparison group of people the same age who had not fallen ill to see if they harbored any kind of S. aureus bacteria. The researchers also tested other members of each patient's household and their social contacts, and took samples from household surfaces to hunt for S. aureus contamination.
In the end, they found evidence that people's homes were "major reservoirs" of a MRSA strain called USA300—which is the chief cause of community MRSA infections across the United States.
Bacteria taken from people living in the same home, for example, were genetically very similar, while there was more genetic variability between samples from different households.
The implication, Uhlemann said, is that "we can't just treat the person with the infection. We have to attempt to remove the (MRSA) colonization from the home."
A MRSA expert who was not involved in the research said it "confirms what we've suspected all along."
"Transmission is a function of contact and time," said Dr. Henry Chambers, chair of the antimicrobial resistance committee for the Infectious Diseases Society of America. "At the end of the day, who are you in contact with the most? Your family."
If you have a MRSA infection, how do you protect your family members? "Basically, it boils down to keeping the wound covered, and frequent hand washing," Chambers said.
According to Uhlemann, you can also use bleach to clean surfaces, and hot water to wash bedding and clothes that an infected person has used. Chambers said the role of surfaces in transmitting MRSA is not "well delineated." But, he added, "it's good to clean."
The U.S. Centers for Disease Control and Prevention estimates about one in three people carries staph bacteria in the nose, usually without sickness. About 2 percent of people harbor MRSA.
It's thought the superbug spread into the wider community because of antibiotic misuse and overuse. When bacteria are exposed to an antibiotic but survive, they can quickly mutate to become resistant to that drug.
Uhlemann's team found some more evidence to point the finger at antibiotic misuse. They discovered that mutations in USA300 that confer resistance to antibiotics called fluoroquinolones (such as ciprofloxacin, sold as Cipro) may have emerged around 1995 in New York City. Fluoroquinolone prescriptions would later soar nationwide—by about 50 percent between 1999 and 2008, the study says.
So it's possible that widespread use of those drugs helped the resistant USA300 strain spread.
"This, once again, argues for the careful use of antibiotics," Uhlemann said.
Chambers agreed. "We know that about half of antibiotics prescribed aren't needed," he said.
Antibiotics kill only bacteria, so they are useless against viral infections such as the common cold and should not be prescribed for those illnesses. If you do need an antibiotic, experts say it's important to take the full course. Stopping too soon could allow some bugs to survive and develop resistance to the drug.
More information: Molecular tracing of the emergence, diversification, and transmission of S. aureus sequence type 8 in a New York community, PNAS, 2014. www.pnas.org/cgi/doi/10.1073/pnas.1401006111
Copyright © 2014 HealthDay. All rights reserved.

















