National AOA Research Fellowship will help shine light on skin cancer
The same enzyme that enables us to walk in the sun without shedding our skin can also enable non-melanoma skin cancer to survive and grow, researchers say.
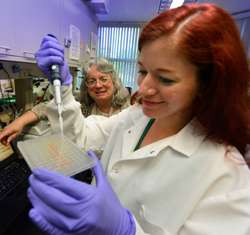
Dr. Abigail Cline, a student at the Medical College of Georgia at Georgia Regents University, is spending the summer between her freshman and sophomore years learning more about the role of this enzyme, protein kinase D, or PKD1, in skin cell damage and death.
Cline is among 50 recipients of the 2014 national Alpha Omega Alpha Carolyn L. Kuckein Student Research Fellowship. AOA, the national honor medical society, awards the fellowships based on the quality and promise of the proposal.
Cline, already a PhD in biochemistry who is contemplating a career in dermatology, considers an early focus on pervasive non-melanoma skin cancers a great place to start. The National Cancer Institute estimates about 2 million new cases this year in the United States.
Non-melanoma skin cancers, which thrive in sun-exposed areas such as the face, can be disfiguring to remove, said Cline's summer mentor, Dr. Wendy Bollag, an MCG cell physiologist who has studied PKD1 for nearly 15 years. "And, just because of the sheer number of cases, even if you just have a small percentage that metastasize, it becomes significant."
Bollag reported in 2010 in the journal Oncogene that ultraviolet light activates PKD1. Her research has also shown that UV's effects are cumulative and dose dependent so more UV exposure equals more PKD1 activity. Resulting problems, including non-melanoma skin cancer, become a particular concern for an aging population.
One of PKD1's many diverse roles in the skin appears to be protecting cells from death, which is great when it means skin cells can survive an afternoon outside. PKD1 also gives cells a better opportunity to recover from minor sun damage.
The tradeoff is that it also can enable badly damaged cells, which will never again serve their original purpose, to avoid natural self-destruction, called apoptosis, and become skin cancer. "It protects them to a fault," said Cline. Increased sun exposure increases the chance of this unhealthy survival.
Now Cline and Bollag want to explore whether reduced levels of PKD1 will increase sensitivity – and so destruction – from UV light.
"We think PKD also protects cells from UV damage," Bollag said. "What Abigail is going to be looking at is whether it also helps accelerate UV repair." In the lab, she will shine ultraviolet light on normal skin tissue as well as tissue in which PKD1 is missing from keratinocytes, the most common skin cell type. As a sort of middle ground, she will also use a topical PKD1 inhibitor on normal skin tissue, then see which tissue experiences the most DNA damage and cell death from UV exposure. These are some of the first studies in tissue with the skin architecture intact; previous work has been in skin cells, Bollag notes.
"We are expecting increased damage compared to controls," Cline said. "Ideally we will find that the knockout has a ton of damage and a lot of apoptosis, the inhibitor cream results in less damage, and the control has no damage."
Another double edge is that PKD1 also tends to support cell proliferation rather than differentiation into mature cell types. Even without sun exposure, skin cells are constantly shedding as the body is continuously makes skin cells. However, without differentiation into mature cell types, like keratinocytes, all that proliferation also provides the vigorous growth required by cancer.
Part of the solution may be a topical cream, like the one the researchers are using, that reduces PKD1 activity just a little so that the enzyme can still enable us to walk outside but also will let seriously damaged cells die.
Increased PKD1 expression has been found in the non-melanoma cancer, basal cell carcinoma; the enzyme also has been implicated in other cancers, including pancreatic and prostate.
Cline hopes that her summer with Bollag will shine more light on PKD1's roles and ultimately lead to better skin cancer prevention and treatment.

















