From knife, to needle, to nothing at all, ultrasound offers the potential for completely bloodless surgery
From knife, to needle, to nothing at all, ultrasound offers the potential for completely bloodless surgery.
The patient, ready to have a malignant breast tumour removed, lies face down on a special operating table with a controlled integrated container of water. The water is the medium through which the surgery will be conducted.
Through an opening in the operating table, the affected breast, inside a latex shield, is suspended in the water. An instrument array comprising multiple robotically operated ultrasound transducers fires up under the guidance of the surgeon.
Using previously determined coordinates, the array precisely targets the cancer deep within the breast tissue. Within seconds the soundwaves travel through the water, unimpaired by air (which disperses sound) and converge, converting their energy to heat that sears away the cancerous tissue. The ultrasound transducers repeatedly refocus and refire, as directed, until all of the identified cancer tissue has been burned away.
These ultrasound waves are tightly focused so that no surrounding tissue is damaged.
There are no cuts, no wounds to heal, no blood loss and no extended hospital stay.
This scenario, while not yet an actual clinical practice, is a realistic glimpse into the future of surgery being designed by Monash University systems engineer Professor Sunita Chauhan, a specialist in medical robotics.
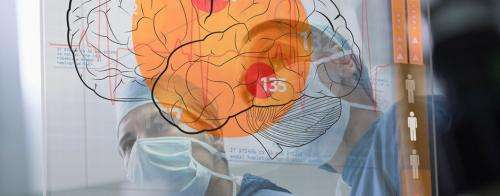
Brain surgery
The type of high-intensity focused ultrasound (HIFU) unit described is still experimental, although a prototype has been developed and patents filed. As spectacular as it already sounds, it is only part of a suite of robotic surgery technologies being researched to finesse procedures and alleviate the trauma of conventional surgery. Professor Chauhan has a particular interest in developing neurosurgery that does not involve cutting into the brain, or even opening the skull.
"If there is one part of the body most in need of the precision of a robotic approach it is the critical brain systems," she says. "Operating in this area presents the highest degree of difficulty for the surgeon in avoiding any damage to critical structures."
HIFU robotic neurosurgery was the subject of Professor Chauhan's PhD at the Imperial College London in 1999. She has been working to make that research a reality ever since. Beginning with Focused Ultrasound Robots, nicknamed FUSBOTs, she has been working on trans-abdominal organs, such as the liver and kidneys, to demonstrate the technology works and is a serious advance in surgical practices. HIFU continues the momentum of minimally invasive surgery that has significantly improved patient outcomes in recent decades. Laparoscopic, or keyhole, surgery uses smaller incisions than traditional surgery and remotely guided equipment. There is reduced blood loss, less pain, fewer complications, a shorter hospital stay and faster recovery than with traditional surgery.
The benefits of robotic systems that provide even greater precision and instrument control have already been demonstrated. One study in Cambridge, UK, showed hospital stays for radical prostatectomies were reduced from an average of 4.9 days for traditional open surgery to 2.8 days following laparoscopic procedures. This was further reduced to 1.3 days with a combination of robotically assisted surgery and post-operative care.
No scalpels
HIFU techniques create the possibility of surgery without a scalpel, reducing the potential for complications inherent in any procedure that cuts into the body. However, most HIFU treatments are still considered experimental.
"It is usually offered to patients who have no alternatives," Professor Chauhan says.
"Some people do not want to have surgery and others are poor candidates for various reasons – their health, or their age. Some people might require multiple surgeries and you can't operate on the same place over and over again because of the scar tissue. Or they might be offered this technique when other treatments, such as radiotherapy, have failed."
She says that, while ultrasound is already used for diagnostic imaging and therapeutic purposes, the potential of HIFU in clinical medicine as a surgical technique is only just beginning to be realised. In procedures such as lithotripsy, ultrasound is used as an alternative to laser or electromagnetic waves to break up gallstones or kidney stones. The fragments are subsequently excreted naturally, avoiding the need for open surgery.
HIFU, which uses precisely targeted soundwaves oscillating at up to 4000 kilohertz, has gradually gained acceptance in procedures to remove benign tumours in the uterus (uterine fibroids), and for tumours associated with prostate cancer. There are already several commercial devices approved for these procedures by the US Food and Drug Administration.
Professor Chauhan says the FUSBOTs she has developed for breast and prostate cancer have now been extended to the treatment of other organs, including the liver and kidneys. But one of the challenges in operating in the trans-abdominal region has been addressing the involuntary movement of these organs in response to respiration and heartbeat.
"Although we have very high-accuracy, high-precision systems delivering the ultrasound, it is difficult to maintain that level of precision when you are targeting something that moves inside," she says. "And this movement can be very unpredictable. In the same person the two kidneys will have completely different patterns of movement, particularly if one is diseased."
Professor Chauhan led a clinical study at the Singapore General Hospital to help understand and quantify the 3-D movement of the kidneys. The trials involved 100 participants – both renal patients and healthy volunteers. The results have helped to identify the ways in which the organs move under both healthy and diseased conditions.
Mannequin patient
In modelling organ movement, Professor Chauhan has been inspired by "Harvey" – the cardiopulmonary mannequin that has become the worldwide medical student training model – to develop her own robotic, smart mannequin patient able to simulate organ movements.
It will help non-invasive robotic systems such as ultrasound, radiosurgery and laser surgery to "learn" about the potential movements of different organs and factor this into their operating systems. Models of the lungs, liver, brain and heart have already been completed; kidneys are next on the list.
"Our smart mannequin project will help to train the surgeons and robotic systems for better treatment outcomes, and will also save the lives of thousands of animals that would otherwise be used for testing."
For Professor Chauhan, much of this work leads back to her initial priority of treating brain tumours. The most common sufferers of brain tumours are children and the elderly – two groups who are also high-risk candidates for conventional neurosurgery. Parts of the brain are also extremely high risk for surgery in terms of the potential for damage to cognitive and motor functions; these areas can, however, be precisely targeted with robotically assisted HIFU.
Fundamental research is continuing into the mechanisms of ultrasound transmission through multi-layered brain structures, and imaging techniques to ensure the most accurate and safest targeting of lesions in the brain.
"But we've still a long way to go," Professor Chauhan says. "We are still working to prove our techniques in non-critical surgeries, before we advance to the brain – our ultimate goal."
















