Cancer researchers use supercomputer to gain insight into new treatment technology
Cancer radiation treatment is a tricky process. Medical researchers and physicians must walk the delicate line of delivering just enough radiation to kill tumors while sparing surrounding healthy tissue.
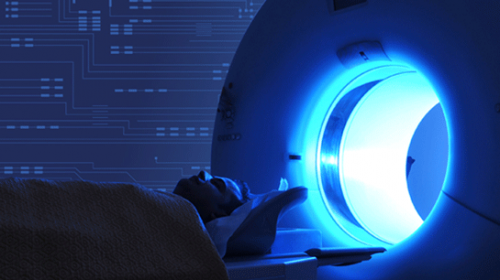
Current radiation treatment relies on imaging from computed tomography (CT) scans, which are taken prior to treatment to determine the tumor's location. This method works fairly well if the tumor lies in an easily detectable and immobile location.
But let's say a patient has lung cancer and will soon undergo radiation treatment. CT scans do not provide real-time imaging of the tumor and in this case, the tumor is constantly moving due to the patient's breathing. The doctor might end up irradiating a large portion of the lung unnecessarily, which could destroy the tumor, but could also lead to a lower quality of life due to effects like difficulty breathing and reduced mobility.
One group, the Elekta and Philips Research Consortium on MRI-Guided Radiation Therapy, is tackling this issue by developing a potentially significant improvement over current technology, the MRI-linac.
The new system unites radiation therapy and magnetic resonance imaging (MRI), allowing physicians to view the tumor in real-time and in high detail during treatment. It also permits physicians to adapt the radiation treatment during the procedure, sparing healthy tissue and reducing side effects.
Like putting together a complicated puzzle, building the MRI-linac relies on many pieces. The research consortium comprises corporations, hospitals, universities, and research institutions worldwide, all of which contribute the distinct research components necessary to develop this technology.
As part of a checks and balances system, one research project at the MD Anderson Cancer Center in Houston focuses on dosimetry—tracking how much radiation is being delivered through the new radiotherapy device.
"Precise knowledge of dose is critical to effective radiation treatment," said Michelle Mathis, a medical physics researcher for the MD Anderson dosimetry team.
"Different tumors need different doses to be killed," Mathis said. "Our work focuses on gaining a better understanding of how to precisely calibrate the new MRI-linac system so that the appropriate amount of radiation is delivered to the cancer tumor while healthy tissue is spared."
Delivering the Right Dose Using Ionization Chambers
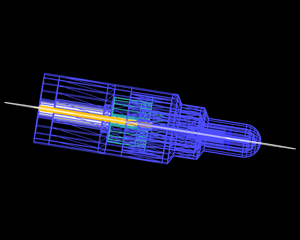
Radiation therapy is typically administered through a linear accelerator, or linac. Inside the linac, electrons are sped up, faster and faster, through an electric field, until they're traveling at nearly the speed of light. Once the electrons reach this speed they hit a target, creating radiation. The radiation is then shaped in the linac, and sprayed down to target the tumor in a patient's body.
Medical physicists use a type of radiation detector called an ionization chamber to ensure that the radiation dose delivered is accurate. Ionization chambers are a necessary part of dose measurement, allowing medical physicists to calibrate the linac.
However, integrating radiation therapy and MRI into a single system adds a magnetic field, which adds a new layer of complication to the performance of ionization chambers.
"In order to adjust for the presence of a magnetic field, we are developing correction factors so that ionization chambers can be used to calibrate the amount of radiation delivered by the new MRI-linac system," Mathis said.
Since only one prototype of the MRI-linac system is available, Mathis performs supercomputer simulations to model radiation in a magnetic field.
The Texas Advanced Computing Center (TACC) at The University of Texas at Austin provides the necessary support to Mathis' research to run these simulations. Through the UT System Research Cyberinfrastructure (UTRC), an initiative that allows any of the 15 University of Texas System institutions access to TACC's supercomputing resources, the team runs simulations on Lonestar, a powerful, high performance computing and remote visualization resource.
"Using Lonestar, we are able to simulate the effect of many variables on the ionization chamber readings, which will allow us to precisely calculate radiation dose," Mathis said.
"Many institutions have their own clusters, however, their machines aren't as powerful or well-maintained as TACC's," said John Fonner, a research associate in TACC's Life Sciences Computing Group. "And because TACC staff are professionals in the advanced computing world, they can provide the technical expertise that other institutions can't, allowing researchers to take their projects to the next level."
The MD Anderson dosimetry team is using a total of 250,000 hours on Lonestar and will continue to run simulations until they can develop correction factors for 16 different ionization chambers.
"By running the supercomputer simulations, our goal is to understand how to properly use ionization chambers in the presence of a magnetic field," Mathis said. "The results of our research will facilitate safe use of the MRI-linac systems, which in turn will be used to treat cancer patients more effectively."
The new MRI-linac has not been released, but the pieces are starting to come together. Several institutions in the consortium have recently been installing initial components. Mathis' dosimetry team will continue working to better understand the system and ensure it functions as intended.
Said Mathis: "Cancer is a global issue, so it's nice to take a holistic approach in improving technology to treat it—ultimately saving more lives and ensuring a better overall quality of life for those affected by cancer."














