Study finds genetic predictor of serious hemorrhagic stroke complications
University of Florida Health researchers have found a possible predictor for little understood—but often disabling or even fatal—stroke complications.
The findings, published today in the journal Proceedings of the National Academy of Sciences, may extend to other neurological disorders, said Sylvain Doré, lead author and a professor of anesthesiology, neurology, psychiatry, pharmaceutics and neuroscience at UF's College of Medicine.
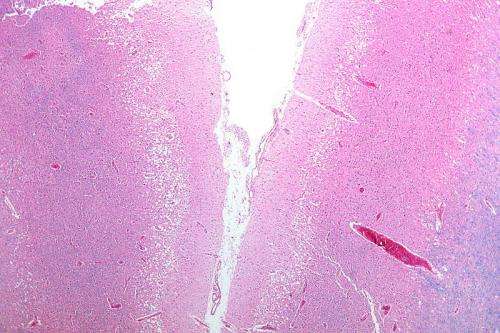
For the study, Doré and his team looked at patients who had suffered a subarachnoid hemorrhage, a type of stroke that affects as many as 30,000 Americans each year and accounts for 5 percent of all strokes, according to the American Heart Association. Most often caused by the rupture of an aneurysm, subarachnoid hemorrhage occurs when there is bleeding in the area between the brain and the thin tissues that cover the brain—often causing death or long-term impairment and disability.
For patients who survive the initial subarachnoid hemorrhagic stroke, two-thirds of them still face a life-threating complication known as cerebral vasospasm, which typically occurs three to 14 days after the initial stroke. The complication occurs when a brain artery temporarily contracts; as a result, the part of the brain formerly supplied by that artery may starve or even die, which causes irreversible brain damage or death.
It's been suggested in the past that one cause of cerebral vasospasm is the compounds within red blood cells, Doré said, which can be released into the brain during rupture of an aneurysm.
"Blood is toxic to the brain," he said. "Every situation where blood goes outside of a blood vessel, it's toxic."
Specifically, the toxic element is hemoglobin, a protein molecule normally tasked with carrying oxygen and iron to the tissues throughout the body. Each red blood cell is capable of releasing 250 million molecules of hemoglobin, so increased levels of toxicity can happen very quickly, Doré said.
However, another molecule traveling throughout the body is haptoglobin, a protein that binds to hemoglobin, helping to nullify its toxic effects—a job it already performs in various organs within the body.
Similar to blood type, each person has one of three haptoglobin phenotypes: Hp1-1, Hp2-1 or Hp2-2. The findings of the study suggest that each phenotype varies in effectiveness when it comes to detoxifying the brain from hemoglobin, and therefore may positively or negatively affect a patient's outcome.
For the study, the researchers analyzed 74 subarachnoid stroke patients and determined each of their the haptoglobin phenotypes, finding that there were no significant differences in terms of age, gender or race among the phenotypes.
However, using brain imaging, a multidisciplinary research team including UF Health vascular neurosurgeon Dr. Spiros Blackburn, found that patients who have the Hp2-2 phenotype were more likely to have suffered cerebral vasospasm after a subarachnoid hemorrhagic stroke than the other groups. They also found that these patients were more likely to have worse outcomes later on.
"Using standard protocols, we see that there's a strong trend at 12 months toward a worse outcome when you are Hp2-2 as compared to the other groups," Doré said.
More research needs to be done with a larger group of study participants to further elaborate on these results, said Jenna Leclerc, an M.D.-Ph.D. student in the department of anesthesiology and neuroscience and a co-author of the study. The team is enrolling patients for further research it hopes will shed light on the specific rolehaptogoblin plays and how it regulates this hemoglobin pathway and potentially reduces cerebral vasospasm, she said.
The team is also interested in improving patient outcomes, either by developing a means to potentially correct or improve the Hp2-2 phenotype or by identifying patients in critical care who have the phenotype.
"The idea is that if we now know there is a subpopulation of patients who have increased risk of complications and mortality, physicians and critical care specialists could potentially monitor those particular patients closer, which would ultimately improve patient outcomes," Doré said.
The team expects the research could also apply to other acute neurological conditions, Leclerc said. "It could be applicable to other types of stroke, as well as various neurological disorders or traumatic brain injuries that cause bleeding in the brain," she said.
More information: Haptoglobin phenotype predicts the development of focal and global cerebral vasospasm and may influence outcomes after aneurysmal subarachnoid hemorrhage, PNAS, www.pnas.org/cgi/doi/10.1073/pnas.1412833112
















