Fast-replicating HIV strains drive inflammation and disease progression
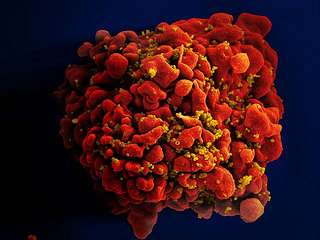
The Human Immunodeficiency Virus (HIV) mutates very rapidly and circulates in many different strains. The strain of HIV someone is first infected with, and its capacity to replicate in the body, can have a lasting influence on how the virus disrupts the immune system, according to a study to be published in Proceedings of the National Academy of Sciences (PNAS).
"These results reinforce our previous findings suggesting that interventions that affect replicative capacity can not only impact disease progression, but also the efficiency of transmission to other people," says senior author Eric Hunter, co-director of the Emory Center for AIDS Research, Georgia Research Alliance Eminent Scholar and a professor of pathology and laboratory medicine at Emory University School of Medicine. "This informs both vaccine development and eradication strategies."
The study team included the Zambia-Emory HIV Research Project (ZEHRP), African researchers supported by Imperial College London and the International AIDS Vaccine Initiative (IAVI), and scientists from the Ragon Institute. The researchers obtained HIV samples from 127 newly infected individuals in Zambia and, for each one, derived a measure of the virus' ability to reproduce in culture. Study volunteers were identified before the provision of antiretroviral therapy, an average of 46 days after the estimated date of infection.
The results confirmed the team's previous finding that the replicative capacity of the newly established virus drives how quickly infected individuals' levels of CD4 T cells declined. CD4 T cell counts are a measure of immune system health and how quickly infected individuals could progress to AIDS. Those infected with poorly replicating viruses progressed to low CD4 T cell counts more than two years after those infected with highly replicating viruses.
However, the new, larger study found that the effect of viral replication capacity was very early after infection, and was independent of both initial viral load and whether individuals carried certain protective variants of immune genes called HLA that positively influence immune responses to HIV. People infected with viruses with high replicative capacity had more signs of acute inflammation in the first few months of infection. Their T cells displayed more signs of "exhaustion," which sets the stage for faster disease progression.
"The effect of viral replicative capacity is just as big as, and independent from, the effect of well-studied protective HLA alleles, which influence whether someone is likely to become an 'elite controller,'" says Daniel Claiborne, lead author and postdoctoral fellow.
"This suggests lowering viral replicative capacity and the resulting immune activation might have benefits, in terms of morbidity and mortality, for individuals whether they remain treatment naïve or go on antiretroviral therapy. This may have important implications for cure strategies aimed at eliminating the viral reservoir, as individuals infected with low replicative capacity viruses may have smaller latent viral pools that may be easier to eradicate. The implication is that if a vaccine enters the fight against HIV, its contribution doesn't have to be a knockout blow. A vaccine that targets qualities of the virus responsible for replicative capacity could have an important impact on disease progression and secondary transmission."
The data come from HIV discordant couples enrolled in ZEHRP as part of IAVI's Protocol C epidemiological study, supported by USAID.
"These findings underscore the huge amount that the HIV vaccine field continues to learn from studies of people in the early, acute states of HIV infection in regions where the epidemic is most severe," says author Jill Gilmour, executive director of IAVI's Human Immunology Laboratory (HIL) at Imperial College London. "The study also illustrates increasing African leadership in HIV vaccine research, a pre-requisite for successful long-term collaborative studies on HIV acute infection to inform vaccine design."
More information: "Selection bias at the heterosexual HIV-1 transmission bottleneck." Science 11 July 2014: DOI: 10.1126/science.1254031
"Replicative fitness of transmitted HIV-1 drives acute immune activation, proviral load in memory CD4+ T cells, and disease progression." PNAS 2015 ; published ahead of print February 17, 2015, DOI: 10.1073/pnas.1421607112
















