X-linked gene mutations cause some cases of male infertility, study says
Some cases of male infertility are due to mutations in the maternal X chromosome that prevent development of viable sperm, according to a study led by researchers at the University of Pittsburgh School of Medicine and the Magee-Womens Research Institute (MWRI). The study was published online today in the New England Journal of Medicine.
Nearly half of cases of male infertility not due to a physical obstruction are estimated to have genetic roots, and about 20 percent of infertile men have azoospermia, meaning they don't make sperm, explained co-principal investigator Alexander Yatsenko, M.D., Ph.D., assistant professor of obstetrics, gynecology and reproductive medicine, Pitt School of Medicine, and an MWRI investigator. He noted the only causes for infertility that have been identified are defects of sex chromosomes, such as the deletions of the Y (male) chromosome or duplication of the entire X (female) chromosome in Klinefelter syndrome.
"Eight times out of 10, conventional genetic testing doesn't reveal a chromosomal problem, so the cause is considered idiopathic or unknown," Dr. Yatsenko said. "This study is among the first to describe specific gene mutations on the X chromosome that contribute to azoospermia and male infertility."
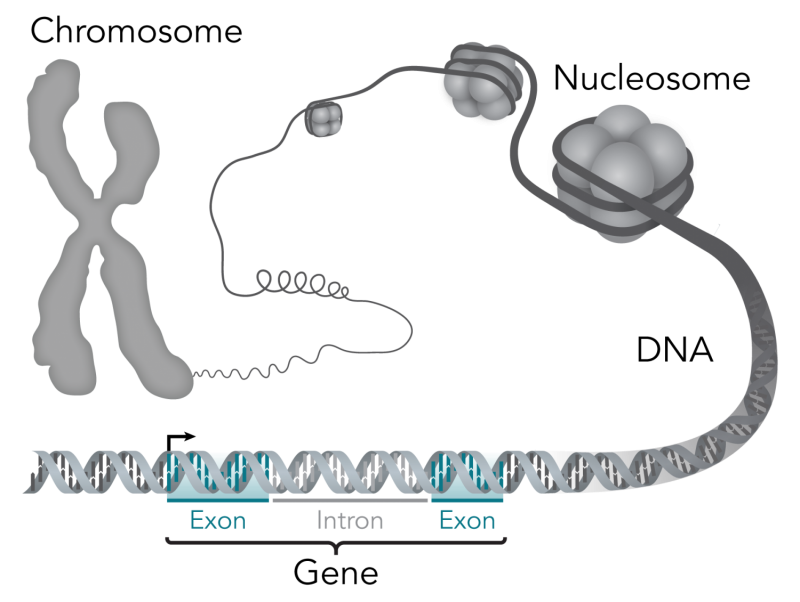
First, the research team scanned the genomes of 15 men with azoospermia and found a deletion in part of the DNA coding of the testis-expressed gene 11 (TEX11) on the X-chromosome, which men inherit from their mothers. The alteration caused meiotic arrest, meaning the precursor cells could not properly undergo meiosis, the cell division process that produces daughter cells with half the parental chromosomes for reproduction.
Then, they found similar TEX11 gene mutations and meiotic arrest in two out of 49 men diagnosed with idiopathic azoospermia from the Center for Fertility and Reproductive Endocrinology at Magee-Womens Hospital of UPMC, and the Institute of Human Genetics of the Polish Academy of Sciences in Poznan, Poland. Also, TEX11 gene errors were found in five out of 240 infertile men from the Center of Reproductive Medicine and Andrology in Münster, Germany.
Dr. Yatsenko noted that it might be possible for an older father, whose precursor sperm cells have a greater likelihood of acquiring a mutation, to pass along the genetic error to his daughter, which could make it impossible for her son to make viable sperm. Also, men without seminal sperm who undergo a procedure to have a few rare, viable sperm extracted from the testes to attempt conception with in vitro fertilization could unknowingly pass a TEX11 gene mutation to a daughter, making her a carrier.
"This research suggests screening for TEX11 gene mutations might be useful in cases of otherwise unexplained azoospermia," Dr. Yatsenko said. "It might be possible to one day correct these problems with gene therapy and other interventions. More work must be done to identify other genetic causes of male infertility."















