Biologists zero in on proteins lumican, TNF-alpha as two-step trigger for deadly scar-tissue production
Scientists at Texas A&M University have made additional progress in understanding the process behind scar-tissue formation and wound healing—specifically, a breakthrough in fibroblast-to-fibrocyte signaling involving two key proteins that work together to promote fibrocyte differentiation to lethal excess—that could lead to new advances in treating and preventing fibrotic disease.
A new study led by biologists Richard Gomer and Darrell Pilling and involving Texas A&M graduate students Nehemiah Cox and Rice University technician Varsha Vakil points to a naturally occurring blood protein, lumican, that, when stimulated by a fibrocyte-secreted protein called tumor necrosis factor alpha (TNF-alpha), triggers a vicious cycle causing inappropriate and uncontrolled formation of scar tissue in fibrotic diseases. Their work, funded by the National Institutes of Health, is published in the current issue of the Proceedings of the National Academy of Sciences.
Fibrotic diseases occur when the body's natural healing mechanisms malfunction and create excessive scar tissue in vital organs, to the point that it becomes harmful. These diseases are wide-ranging—lung, kidney, liver and heart fibrosis are some of the most common—and are associated with 45 percent of U.S. deaths per year.
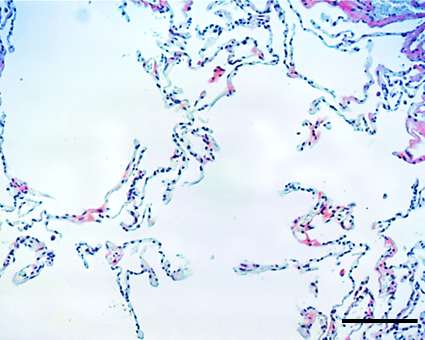
For their analysis, Gomer and Pilling examined the lung tissue of human patients with pulmonary fibrosis and observed the presence of lumican. In patients with relatively normal lung function, the lumican was present at lower levels, whereas it was more prevalent in patients in advanced stages of the disease.
"Our data suggests that lumican may be one of the unknown signals from fibroblasts to fibrocytes that controls part of a runaway feedback loop that encourages fibrosis," Gomer said. "Therefore, lumican-inhibiting drugs may prove useful as possible therapeutic treatments for fibrosis."
Gomer and Pilling, who joined the Texas A&M Department of Biology in 2010, were able to show in previous studies that bacteria-fighting white blood cells called monocytes enter fibrotic lesions and develop into wound-healing fibrocytes, which are cells that help to mediate tissue repair. Researchers have theorized that the development of fibrosis may involve a miscommunication between fibrocytes and fibroblasts, the main cells that form scar tissue.
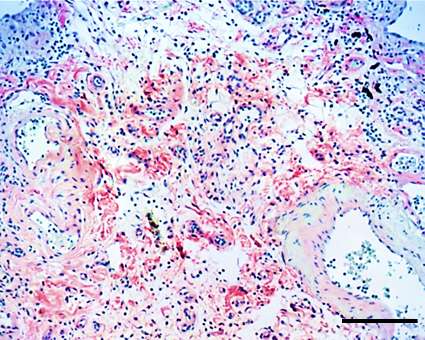
In their most recent work, Gomer and Pilling zeroed in on TNF-alpha as a possible source of the miscommunication. While fibroblasts naturally only produce a small amount of lumican, TNF-alpha stimulates them to produce even more lumican during scar formation. The excessive lumican triggers monocytes, which can differentiate to play multiple roles in immune-system function, to become fibrocytes—a transformation that results in additional TNF-alpha production that, in turn, triggers increased lumican production. Ultimately, this leads to an overabundance of scar tissue in the lungs, a process called a positive feedback loop.
"This research may help explain why fibrosis persists, why it is difficult to treat, and may suggest new methods to treat fibrosis," Pilling said.
Fibrotic diseases and potential treatments have become a hot talking point in biomedical circles in recent years, and both Gomer and Pilling have become nationally recognized as preeminent authorities on fibrotic research.
In the early 2000s, the two identified another naturally occurring blood protein called serum amyloid P, or SAP, as a signal that inhibits the formation of fibrocytes. By 2006, their work to harness SAP's wound healing capabilities had progressed to the point that they co-founded a company, Promedior Inc., to further develop SAP-related technology.
Their first major breakthrough came in 2007, when they and colleagues found that SAP is effective at preventing fibrotic disease in the lungs and hearts of laboratory animals. In 2013 and 2014, Promedior announced that early clinical trials of a treatment involving a recombinant form of SAP, PRM-151, indicated a successful reduction of symptoms in patients with lung fibrosis and myelofibrosis, a life-threatening scarring of bone marrow.
On Aug. 31, New York-based global biopharmaceutical company Bristol-Myers Squibb announced an agreement to give Promedior $150 million to fund further clinical trials and potentially to acquire Promedior for up to $1.25 billion.
"We are obviously delighted that Bristol-Myers Squibb is supporting the work to break the vicious cycle in fibrosis and thus help patients with fibrosing diseases," Gomer said.
From identifying SAP as the protein that inhibits scar-tissue formation to investigating its direct competition, lumican, as the protein that promotes it, Gomer says the real winner in his and Pilling's ongoing research is the patient.
"It looks like SAP rules them all," Gomer said. "The proof of the pudding is that SAP treatments cause patients to improve, not just stabilize. So to our delight, it looks like SAP is a dominant factor."
More information: TNF-α–stimulated fibroblasts secrete lumican to promote fibrocyte differentiation, www.pnas.org/cgi/doi/10.1073/pnas.1507387112















