New neuroimaging method better identifies epileptic lesions
Epilepsy affects more than 65 million people worldwide. One-third of these patients have seizures that are not controlled by medications. In addition, one-third have brain lesions, the hallmark of the disease, which cannot be located by conventional imaging methods. Researchers at the Perelman School of Medicine at the University of Pennsylvania have piloted a new method using advanced noninvasive neuroimaging to recognize the neurotransmitter glutamate, thought to be the culprit in the most common form of medication-resistant epilepsy. Their work is published today in Science Translational Medicine.
Glutamate is an amino acid which transmits signals from neuron to neuron, telling them when to fire. Glutamate normally docks with the neuron, gives it the signal to fire and is swiftly cleared. In patients with epilepsy, stroke and possibly ALS, the glutamate is not cleared, leaving the neuron overwhelmed with messages and in a toxic state of prolonged excitation.
In localization-related epilepsy, the most common form of medication-resistant epilepsy, seizures are generated in a focused section of the brain; in 65 percent of patients, this occurs in the temporal lobe. Removal of the seizure-generating region of the temporal lobe, guided by preoperative MRI, can offer a cure. However, a third of these patients have no identified abnormality on conventional imaging studies and, therefore, more limited surgical options.
"Identification of the brain region generating seizures in location-related epilepsy is associated with significantly increased chance of seizure freedom after surgery," said the new study's lead author, Kathryn Davis, MD, MSTR, an assistant professor of Neurology at Penn. "The aim of the study was to investigate whether a novel imaging method, developed at Penn, could use glutamate to localize and identify the epileptic lesions and map epileptic networks in these most challenging patients."
"We theorized that if we could develop a technique which allows us to track the path of and make noninvasive measurements of glutamate in the brain, we would be able to better identify the brain lesions and epileptic foci that current methods miss," said senior author Ravinder Reddy, PhD, a professor of Radiology and director of Penn's Center for Magnetic Resonance and Optical Imaging.
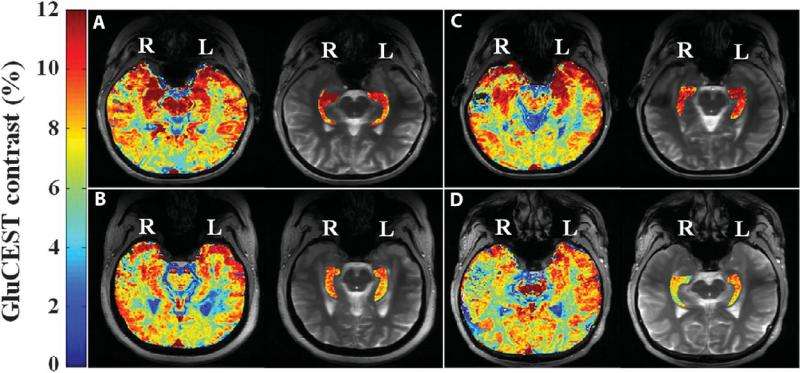
Reddy's lab developed the glutamate chemical exchange saturation transfer (GluCEST) imaging method, a very high resolution magnetic resonance imaging contrast method not available before now, to measure how much glutamate was in different regions of the brain including the hippocampi, two structures within the left and right temporal lobes responsible for short- and long-term memory and spatial navigation and the most frequent seizure onset region in adult epilepsy patients.
The study tested four patients with medication-resistant epilepsy and 11 controls. In all four patients, concentrations of glutamate were found to be higher in one of the hippocampi, and confirmatory methods (electroencephalography and magnetic resonance spectra) verified independently that the hippocampus with the elevated glutamate was located in the same hemisphere as the epileptic focus/lesion. Consistent lateralization to one side was not seen in the control group.
While preliminary, this work indicates the ability of GluCEST to detect asymmetrical hippocampal glutamate levels in patients thought to have nonlesional temporal lobe epilepsy. The authors say this approach could reduce the need for invasive intracranial monitoring, which is often associated with complications, morbidity risk, and added expense.
"This demonstration that GluCEST can localize small brain hot spots of high glutamate levels is a promising first step in our research," Davis said. "By finding the epileptic foci in more patients, this approach could guide clinicians toward the best therapy for these patients, which could translate to a higher rate of successful surgeries and improved outcomes from surgery or other therapies in this difficult disease."
More information: Glutamate imaging (GluCEST) lateralizes epileptic foci in nonlesional temporal lobe epilepsy, Science Translational Medicine, stm.sciencemag.org/lookup/doi/ … scitranslmed.aaa7095















