Viral infections leave a signature on human immune system, study finds
A team of immunologists and informatics experts at the Stanford University School of Medicine has identified a distinctive pattern of gene expression that distinguishes people with a viral infection from those with a bacterial infection. The team also identified a second pattern of gene expression that is more specific: It can distinguish the flu from other respiratory infections.
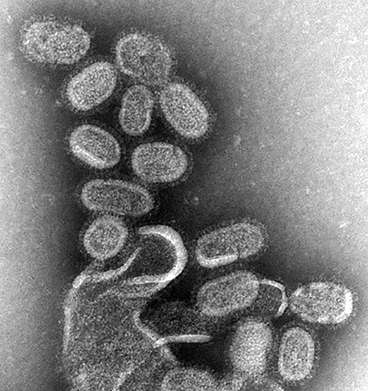
When pathogens infect the cells of the body, the infection sets off a chain reaction involving the immune system that changes the expression of hundreds of genes. Gene expression is the process by which cells extract information from the genes and render it as molecules of protein or RNA. Cells have the capacity to express more or less of each molecule, creating a pattern of expression that changes in response to external influences—including infection by viruses.
Purvesh Khatri, PhD, assistant professor of medicine, and a team of six other researchers at Stanford identified 396 human genes whose expression changes in a consistent pattern that reveals the presence of a viral infection. The pattern of changes, which they call the meta-virus signature, occurs in a range of viruses and is distinct from the pattern of gene expression in healthy people or in people with bacterial infections. The meta-virus signature pattern of gene expression is also present even before a person has clear symptoms of infection.
In their paper, to be published Dec. 15 in Immunity, the authors also described a second gene expression pattern that signals when a person is infected specifically with the flu virus. This second pattern, the influenza meta-signature, consists of a change in the expression of just 11 human genes. The influenza meta-signature pattern can distinguish flu from other viral infections, as well as from bacterial infections. It can also identify a flu infection before a person has symptoms and even reveal whether a person is building immunity after getting the flu vaccine.
Khatri, a bioinformatician, is the senior author of the paper. Lead authorship is shared by doctoral student Marta Andres-Terre and former postdoctoral scholar Helen McGuire, PhD.
Khatri said his team was motivated by the long-term goal of finding broad-spectrum antiviral drugs, much like the broad-spectrum antibiotics that have saved so many people from deadly bacterial infections. Broad-spectrum antivirals could be used against dengue fever and other killers, he said.
Waving a red 'infection' flag
The researchers' first step was to look for a general change in gene expression in response to infection by viruses generally. They began by looking at changes in gene expression in a set of publicly available data. In blood samples from 205 people infected with a flu, cold or respiratory syncytial virus, the team found 396 genes whose expression changed in the same way during all three types of infections, with an increase in the expression of 161 genes and a decrease in the expression of 235 genes.
The team then found the same pattern in a larger group of blood and tissue cell samples from 2,939 people consisting of healthy controls and those infected with a diverse array of pathogens, including viruses such as SARS coronavirus, enterovirus and adenovirus, as well as bacteria such as Escherichia coli, Staphylococcus aureus, Streptococcus pneumoniae and Salmonella. In the larger group, the team found the same altered pattern of expression in the same 396 genes among patients with viral infections.
The meta-virus signature not only identified individuals with an active viral infection, but also those who were incubating one. By studying blood samples taken frequently—every eight hours for five days—the Stanford team discovered the meta-virus signature pattern waving a red "infection" flag up to 24 hours before the first symptoms. "An individual's gene expression signature changed before they became sick, so we could predict up to 24 hours before who was going to show symptoms," said Khatri.
The same high-frequency sampling data also revealed that the meta-virus signature signal, the one indicating any virus, began first. Then, a few hours later, the more-specific influenza meta-signature signal began in people with the flu. "It seems that when there is a viral infection, the immune system turns on a general response to all viruses, followed by a virus-specific response to the particular virus," said Khatri. "You can imagine a decision tree where the immune system asks, 'Is it bacterial or viral?' And if it's viral it turns on the meta-virus signature response. And then it asks, 'If it's viral, which virus is it?' And then it turns on a specialized response for that virus."
Theoretically, the meta-virus signature could be used clinically to distinguish viral from bacterial infections to determine if an antibiotic should be prescribed. The Khatri lab has funding to develop such a test.
The team's work is an example of Stanford Medicine's focus on precision health, the goal of which is to anticipate and prevent disease in the healthy and precisely diagnose and treat disease in the ill.
Is the vaccine working?
The work can also help determine whether someone is responding to vaccination. "The goal of vaccination is to generate the same immune response without the symptoms," he said. "If the IMS response is truly virus-specific, we should see the same response in vaccination." And, in fact, the Khatri team found that in three independent studies of flu vaccine recipients, all those judged to have responded to vaccination by other measures also displayed the 11-gene influenza meta-signature. Likewise, nonrespondents showed no influenza meta-signature response. In short, if you see the gene expression signature, you know the person is responding to the vaccine.
Until now, said Khatri, no one has found the immune response that turns on in both the vaccination response and in actual infections. This paper demonstrates for the first time a "transcriptional signature" that can be used as a proxy for whatever immune mechanism is induced by both vaccination and infection. "We have identified the common signature that links infection and vaccination," he said.
The work on the vaccination response also added to the understanding of men's immune response, which is different from women's. Other research has suggested that men's immune response to vaccines was somehow suppressed. In previous work, researchers looked at men's and women's responses on the third day after vaccination, when women had a strong reaction and men had none. But Khatri's group found that men were responding most on the first day after vaccination. In other words, men were responding to flu vaccine sooner than women. By the third day, men's immune response returned to baseline. "The dynamics are different," he said, "and we haven't been sampling at the right time."
The Stanford paper also looked at samples from patients with acute pneumonia. In these patients, the influenza meta-signature distinguished viral pneumonia from bacterial pneumonia. As patients recovered, their influenza meta-signatures gradually returned to a healthy baseline level. "So you can also use IMS to monitor patients' progress," said Khatri.



















