Discovery could help treatments for sickle cell disease
An interdisciplinary, international group of researchers has found new biophysical markers that could help improve the understanding of treatments for sickle cell disease, a step toward developing better methods for treating the inherited blood disorder that affects an estimated 80,000 to 100,000 Americans each year.
"There is a critical need for patient-specific biomarkers that can be used to assess the effectiveness of treatments for sickle cell disease," said Subra Suresh, president of Carnegie Mellon University and co-author of the study. "This study shows how techniques commonly used in engineering and physics can help us to better understand how the red blood cells in people with sickle cell disease react to treatment, which could lead to improved diagnostics and therapies."
The findings from engineers, physicists and clinicians from Carnegie Mellon, the University of Pittsburgh, the Massachusetts Institute of Technology, Florida Atlantic University, Korea University, the Korea Advanced Institute of Science and Technology, and Harvard University will be published this week in the online early edition of the Proceedings of the National Academy of Sciences (PNAS).
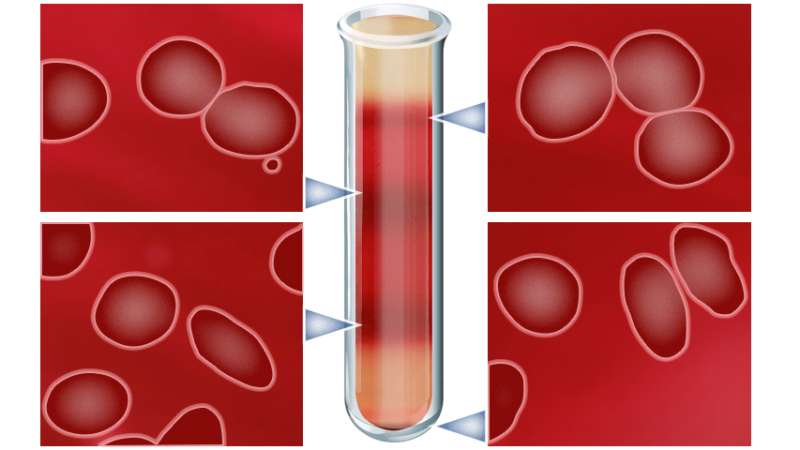
People with sickle cell disease have an abnormal form of hemoglobin, a protein found in red blood cells that carry oxygen throughout the body. Normal red blood cells are flexible discs that easily bend and stretch to flow through the body's narrow blood vessels. In sickle cell disease, the abnormal hemoglobin forms fibers that cause the blood cells to take on a flattened, sickled shape and stiffen when they lose oxygen. This change in shape and rigidity causes the red blood cells to be stuck in the blood vessels and prevents the transport of oxygen to the surrounding tissue. This can cause anemia and extreme pain and impact the health of the body's tissue and organs.
Currently, hydroxyurea is the only FDA-approved drug for sickle cell disease. The drug reduces sickling in red blood cells and is used to treat pain and reduce the need for blood transfusions in some patients, but it does not work in all patients. Researchers have been divided over what mechanisms cause the drug to work. Some believe it works by reactivating fetal hemoglobin, which is better at transporting oxygen than the abnormal hemoglobin that causes sickling. Others believe it works by increasing the volume of red blood cells, reducing the concentration of sickle hemoglobin.
In the current study, the international research team evaluated the biophysical properties—shape, surface area and volume—and biomechanical properties—flexibility and stickiness—of red blood cells under normal oxygenated conditions using electromagnetic waves to measure small differences in physical properties. The technique, known as common-path interferometric microscopy, allowed researchers to get a three-dimensional view of the cells.
Using blood samples from patients with sickle cell disease, the researchers separated red blood cells into four groups based on their density. Normal, disc-shaped red blood cells were the least dense, while severely sickled cells were the most dense. They then took samples from people receiving hydroxyurea treatment and those not receiving treatment. The red blood cells of those receiving treatment showed an improvement in all of the biophysical and biomechanical properties tested across all density levels. Furthermore, improvement in the physical properties of red blood cells of people treated with hydroxyurea correlated more with an increase in the red blood cell volume than with levels of fetal hemoglobin.
"Our findings shine a light on the mechanism behind hydroxyurea action, which has long been debated in the scientific community," said Ming Dao, principal research scientist in MIT's Department of Materials Science and Engineering and co-author of the study. "It's exciting to see that using the latest optical imaging tools, we can now confirm which one is the dominating mechanism. Understanding the key mechanism of action will allow us to explore novel and improved therapeutic approaches for sickle cell disease."
The researchers hope that these biophysical markers can be combined with biochemical and molecular-level markers to assess things like the severity of a patient's sickle cell disease, determine whether or not a patient will respond to hydroxyurea treatment and monitor the effectiveness of that treatment.
More information: Cellular normoxic biophysical markers of hydroxyurea treatment in sickle cell disease, PNAS, www.pnas.org/cgi/doi/10.1073/pnas.1610435113

















