Nanoparticle drug cocktail could help treat lethal cancers
Cancer treatments that mobilize the body's immune system to fight the disease have generated a lot of excitement in the past few years. One form of immunotherapy called checkpoint blockade is especially promising. But while checkpoint blockade has had some striking successes, the therapy has almost no effect on some of the most lethal kinds of tumors.
Now a group of scientists from the University of Chicago has developed an ingenious way to spur checkpoint blockade into more potent action. The therapy, reported in the Aug. 17 issue of Nature Communications, offers the hope of an effective treatment for intractable metastatic cancers including those of the colon and lung.
"Everybody out there working in the cancer space is trying to figure out ways to enhance checkpoint blockade immunotherapy," said Wenbin Lin, James Franck Professor in Chemistry at UChicago and one of the scientists who conceived the new therapy. "In this work, we were able to achieve that."
The method requires a complex interplay of immune-stimulating nanoparticles comprised of light-sensitive agents and standard chemotherapeutic drugs, both acting together to fortify the checkpoint blockade.
Bolstering immunity
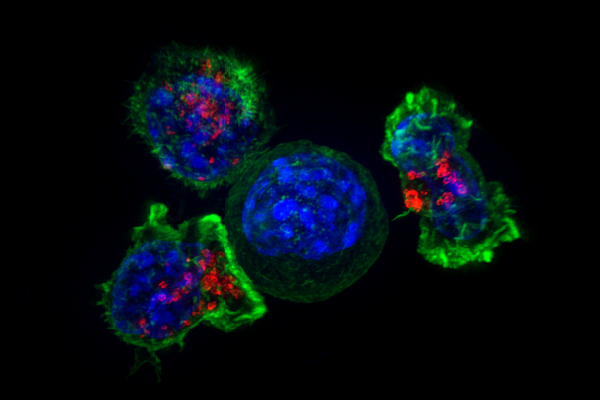
Checkpoint blockade therapy works by interfering with cancer's ability to turn off the body's immune reaction. When cancer cells first develop, the body is able to recognize them as foreign, triggering T-cells to attack and eliminate them. But as malignant cells multiply and form tumors, they release biochemical signals that suppress the immune system and the T-cells no longer function properly.
Checkpoint blockade therapy obstructs those signals, makes T-cells see the cancer cells as invaders again, and allows the immune system to do its job. The problem, said Lin, is that if a tumor has been growing for years there are no longer any T-cells inside it to activate, so the therapy fails.
"So what we're trying to do is to come up with ways to recruit T-cells to the tumor," he said. "And if you have a way to make the T-cells recognize cancer cells, the T-cell will be able to go in there and kill the cancer cells."
The treatment Lin and collaborators invented is a drug cocktail contained in a nanoparticle. The nanoparticles assemble themselves from zinc and a drug called oxaliplatin, which is widely used against advanced-stage metastatic colon cancer. A photosensitizing agent called pyrolipid forms the outer layer. When light is shined on the pyrolipid it generates molecules that can kill cancer. It also activates T-cells that can recognize cancer cells, so the nanoparticles pack a triple punch.
Used in concert, the nanoparticles and a checkpoint blockade agent were able to eliminate tumors in a mouse, even when the tumors were widely separated and one of them had received no treatment. The scientists injected a checkpoint blockade drug into the abdomen of a mouse that had two tumors growing at different places on its body, and then injected the nanoparticles into the mouse's tail vein. They shined light onto one of the tumors to activate the pyrolipid. The other tumor was left untreated.
The irradiated tumor disappeared, as would be expected. But, remarkably, the distant, untreated tumor disappeared as well. No irradiation with light meant no T-cells were activated in the second tumor, "so we should not expect that tumor to disappear," Lin said. "But we believe that this combination is able to activate the immune system to generate the T-cells that will recognize the cancer cells. Then they go around the body and kill the cancer cells in the distant site that has not been irradiated with the light."
Traveling T-cells
This ability to activate T-cells in one place and have them travel to disease sites elsewhere in the body could be a powerful tool for treating cancer. Most people who die of cancer do not die from their primary tumor; they die from metastatic disease. When patients have surgery, surgeons don't know if there are other, smaller lesions elsewhere in the body.
"You cannot treat them because you don't know where to look for them," Lin said. "If you activate immune cells, they can home in to cancer cells selectively. So you have a better chance of getting rid of these small metastatic tumors throughout the body."
Lin and colleagues have started a company to develop the new therapy and have raised initial funding for clinical trials.
"These findings open up new opportunities for using nanoparticles as a platform for combination therapies," said Yu-Ying He, an associate professor of medicine and dermatology at UChicago who is familiar with the work. "If the mouse models are indicative of human disease, the combination therapy can increase the proportion of patients who respond to therapy without additional adverse side effects and can improve the quality of life for cancer patients."
More information: Chunbai He et al. Core-shell nanoscale coordination polymers combine chemotherapy and photodynamic therapy to potentiate checkpoint blockade cancer immunotherapy, Nature Communications (2016). DOI: 10.1038/ncomms12499
















