Last-line antibiotics are failing
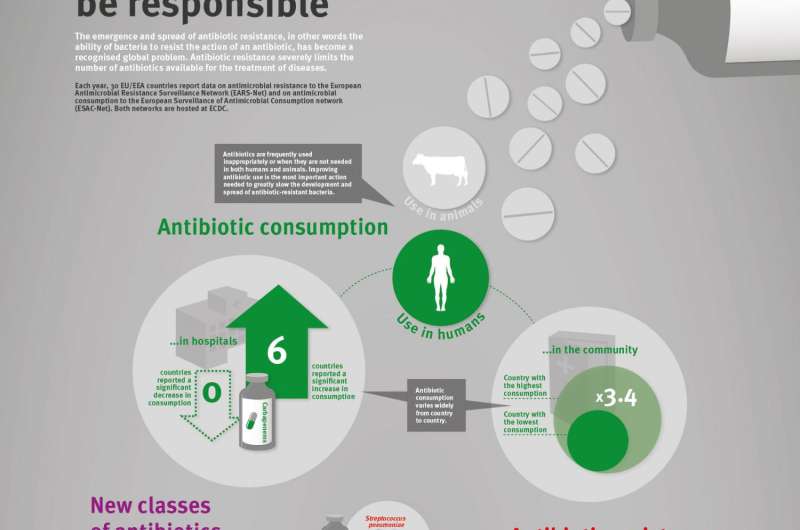
On the occasion of the 9th European Antibiotic Awareness Day, the European Centre for Disease Prevention and Control (ECDC) is releasing its latest EU-wide data on antibiotic resistance and antibiotic consumption. In 2015, antibiotic resistance continued to increase for most bacteria and antibiotics under surveillance. In particular, the EU average percentage of carbapenem resistance in Klebsiella pneumoniae increased from 6.2% in 2012 to 8.1% in 2015, and combined resistance to carbapenems and polymyxins (e.g. colistin) was sometimes reported. These two groups of antibiotics are considered last-line antibiotics as they usually are the last treatment options for patients infected with bacteria resistant to other available antibiotics. While antibiotic consumption in hospitals significantly increased in several EU Member States, antibiotic consumption in the community decreased in six EU Member States.
Vytenis Andriukaitis, European Commissioner for Health and Food Safety, said: "Antibiotic resistance is one of the most pressing public health issues of our time. If we don't tackle it, we can go back to a time when even the simplest medical operations were not possible, and organ transplants, cancer chemotherapy or intensive care even less so". He added: "The European Commission will launch a new Action Plan next year so that we can, together with our partners in the EU Member States and internationally, continue to ensure that the prevention and control of antibiotic resistance is strengthened within a one-health approach".
ECDC Acting Director, Dr Andrea Ammon, said: "Antibiotic resistance in Klebsiella pneumoniae is of increasing concern in Europe. More than one third of the isolates reported to ECDC for 2015 were resistant to at least one of the antibiotic groups under surveillance, and combined resistance to multiple antibiotic groups was common. Moreover, the emergence of K. pneumoniae infections with combined resistance to carbapenems and colistin is worrisome and an important warning that options for treatment are now even more limited than in the past". Dr Ammon added: "However, the decrease of antibiotic consumption in the community in six countries is a positive sign and shows that we are starting to use antibiotics more prudently. Prudent use of antibiotics is pivotal, both in the community and in hospitals, to ensure that these drugs remain effective".
ECDC's data also show that antibiotic resistance in Escherichia coli, one of the most frequent causes of bloodstream infections and community- and healthcare-associated urinary tract infections, requires close attention as the percentages of isolates resistant to commonly used antibiotics continues to increase throughout Europe. In contrast, the percentage of meticillin-resistant Staphylococcus aureus (MRSA) showed a significantly decreasing trend at EU/EEA level between 2012 and 2015. Despite this positive development, MRSA remains a public health priority as eight out of thirty countries reported percentages above 25%.
Dr Zsuzsanna Jakab, WHO Regional Director for Europe said: "Surveillance of antibiotic resistance is the backbone of our work in defence of antibiotics' effectiveness. Until we know where resistance is, we cannot prioritize action. This is why we focus on expanding the map of antibiotic resistance beyond the European Union countries through the Central Asian and Eastern European Surveillance of Antimicrobial Resistance (CAESAR) network. What the report indicates is of concern: our patients are exposed to resistant bacteria in hospitals due to overuse and misuse of antibiotics and poor infection prevention and control. We urge our leaders to use this evidence and accelerate their response to a major global health threat of our time".
Activities promoting prudent use of antibiotics are organised in more than 40 countries across the European Region during the week of 18 November to mark European Antibiotic Awareness Day. ECDC works jointly with the World Health Organization (WHO) Regional Office for Europe, and partners World Antibiotic Awareness Week.
ECDC, in cooperation with the European Commission, will host an EU-level launch event entitled "European Antibiotic Awareness Day: the future is now". The planned interventions will not only present the current situation and future steps at EU level, but will also aim at highlighting how resistance to antibiotics is affecting our lives today and what can be done by different sectors to ensure that they remain effective. It will take place on 18 November 2016, from 9:30 to 13:00 CET, and will be web streamed here: http://bit.ly/2f7IgiQ. ECDC and partner organisations will be live tweeting from the event using #EAAD2016.
Following the success of last year's 24-hour Global Twitter conversation on antibiotic resistance and prudent use of antibiotics around the world, ECDC is again coordinating a Global Twitter conversation on 18 November, hosted jointly by participating organisations from Australia, Canada, New Zealand, the United States, and WHO Headquarters and the WHO Regional Offices. The hashtags that will be used are #AntibioticResistance and #EAAD2016.















