Hepatitis B and C can be wiped out in the US by 2030; here's how
Health experts have devised an aggressive plan to stamp out a viral disease that is fueling a sharp rise in liver cancer in the United States and killing 20,000 Americans per year.
Their national strategy for eliminating two types of hepatitis by 2030 hinges on persuading the federal government to purchase the rights to one or more of the costly new medications that can essentially cure hepatitis C.
That unprecedented step is one of a raft of recommendations issued Tuesday by the National Academies of Sciences, Engineering, and Medicine. The academies' expert panel also recommended a campaign to vaccinate all adults against hepatitis B, expanding needle exchanges for intravenous drug users and a nationwide effort to identify and treat the legions of Americans who are unknowingly infected with either strain of the virus.
All these efforts should be coordinated by a single federal office, the panel proposed.
With about 2.7 million Americans infected with hepatitis C and 1.3 million people infected with hepatitis B, the stakes are high. A 2009 report estimated that the annual cost to Medicare of caring for hepatitis C patients alone would increase from $5 billion in that year to $30 billion in 2030. And that forecast didn't include a new generation of expensive drugs.
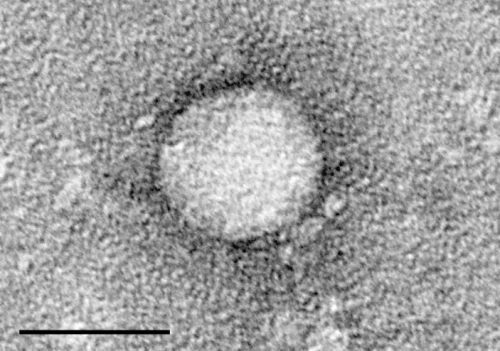
The viruses that cause hepatitis B and C are spread through sexual contact, needle sharing and incidental exposure to infected blood. Most people with the viruses are unaware they are infected, which allows both strains to spread unchecked. Infection rates are especially high among ethnic minorities, prison populations and people who inject drugs. This last group accounts for 75 percent of the roughly 30,500 new hepatitis C infections every year in the United States.
Although infection causes no illness in its early stage, over time both strains can scar the liver, impair its function and give rise to malignancy. The nation's unseen hepatitis epidemic is widely credited with making liver cancer the fastest growing form of malignancy and driving a dramatic increase in liver cancer deaths seen in the last decade. Hepatitis B and C also account for roughly 2,400 liver transplants each year.
The Food and Drug Administration has approved a few new antiviral medications to treat hepatitis C in the last two years. These therapies can completely clear the virus from a patient's body in as little as eight weeks with a single daily pill.
But they haven't been widely used for a single reason: cost. The price for a full course of treatment can range from $55,000 to $150,000. As a result, government insurance programs such as Medicaid and Medicare have limited their use to patients with late-stage disease, and private insurers have imposed onerous copayments, paperwork and delays on patients and their doctors. The panel's experts estimated that by 2015 only 7 percent to 14 percent of patients known to be infected with hepatitis C had started treatment with the new drugs.
These drugs are among the most expensive oral medications in history, and will probably remain so until 2029, when the exclusive patent rights on the first of these new medications expires.
That's why licensing one or more of the new-generation drugs is a key part of the panel's plan. A licensing deal could cost taxpayers an estimated $2 billion, and the medications would then be used to treat government-insured patients whose access is now limited, including 700,000 Medicaid beneficiaries, prison inmates and enrollees in the Indian Health Service.
Such an arrangement could save the United States more than $8 billion by 2030, the panel estimated. Far from disadvantaging the company that agrees to a deal, the move would broaden the reach of its product to patients who would not otherwise be treated, said Rutgers University Chancellor Dr. Brian L. Strom, who chaired the panel.
"It's a win-win for everybody," Strom said Tuesday. "For the public, it's a massive win" that would drive down the number of infected Americans spreading the virus unwittingly. And for at least one of the five drugmakers who manufacture these costly medications (Gilead Sciences, Merck, Bristol-Myers Squibb, AbbVie and Janssen), striking a voluntary licensing agreement could return handsome dividends on its investment in research and development, he added.
The drugs - marketed under such names as Sovaldi, Daklinza, Olysio and Zepatier - "are great products and we certainly wouldn't want to undercut industry's ability" to develop other such medications in the future, Strom said.
While legally allowed, the unconventional step of forging a licensing agreement between a drug manufacturer and the federal government comes at a pivotal moment in politics, medicine and public health.
Enter President Donald Trump, who has said pharmaceutical manufacturers are "getting away with murder" and vowed to lower the cost of medications by negotiating new deals. On March 7, he tweeted, "I am working on a new system where there will be competition in the Drug Industry. Pricing for the American people will come way down!"
The National Academies panel said that nothing short of "unrestricted mass treatment of hepatitis C" will eliminate the disease by 2030. Delays imposed by the treatments' high costs, they added, "would result in tens of thousands of needless deaths and billions of dollars in wasted medical costs" aimed at treating the cancers, cirrhosis and other liver diseases caused by untreated hepatitis C infection.
"There are times when the government must act to correct a market failure," the panel wrote.
Pointing to a 2014 investigation by the Senate Finance Committee, the 17-member panel suggested that deliberate pricing decisions made by Gilead Sciences - the first pharmaceutical to bring a new-generation hepatitis C drug to the market - have inflated the cost not just of its medication, but of all other such drugs to follow.
"Action now might discourage other companies from pursuing this strategy in the future," the panel said.
The committee also said the U.S. could halve the number of annual deaths from hepatitis B by 2030 if it diagnosed 90 percent of the nation's chronic patients, brought 90 percent of those to care, and treated 80 percent of those for whom treatment is warranted. These actions would avert more than 60,000 deaths per year and reduce liver cancer and cirrhosis from hepatitis B infection by about 45 percent.
At the same time, treating everyone with chronic hepatitis C would reduce new infections by 90 percent by 2030 and reduce hepatitis C deaths by 65 percent over the same time. Although the task would grow tougher as cases dwindled, the panel reckoned that such actions would avert 28,800 deaths by 2030.
"Viral hepatitis is simply not a sufficient priority in the United States," Strom said. "Despite being the seventh leading cause of death in the world - and killing more people every year than HIV, road traffic accidents, or diabetes - viral hepatitis accounts for less than 1 percent of the National Institutes of Health research budget."
©2017 Los Angeles Times
Distributed by Tribune Content Agency, LLC.

















