Scientists plot antibiotic resistance on a world map
Russian scientists have created an interactive world map of human gut microbiota with potential to resist antibiotics, known as the resistome. Their ResistoMap will help identify national trends in antibiotic use and control antibiotic resistance on a global scale.
In 2014, the problem of drug resistance was named among serious threats to human health by the World Health Organization (WHO). "Because we are not taking any rapid and coordinated measures, the world is entering an age of diminished antibiotic efficiency, with common infections and minor injuries taking lives—many decades after we learned to treat them successfully," said Keiji Fukuda, who was then the assistant director-general for health, security, and environment of the WHO.
Microbial drug resistance is caused by the extensive, uncontrolled use of antibiotics in medicine and agriculture. It has been predicted that by 2050, around 10 million people will die annually from causes associated with drug resistance. Russian scientists from the Moscow Institute of Physics and Technology have created the ResistoMap (from the Latin word resisto, "I resist"), an interactive visualization of the gut resistome, i.e., the set of all antibiotic resistance genes in the genomes of human gut microbes. The geographic map navigation layer is a feature of the new tool that enables researchers to state hypotheses regarding global trends in antibiotic resistance and correlation of gut resistome variations with the national clinical guidelines on antibiotic use.
What makes microbiota so special?
The human microbiota, also known as the microbiome or microflora, refers to the aggregate of all microorganisms residing in the human body. Compared to other organs, tissues and biofluids, the gut flora has the largest number of bacteria. The latest studies show that gut flora could—in terms of its importance for human health—be viewed as a separate organ composed of a multitude of bacteria, both attached to the intestinal wall and living in the intestinal lumen. Although invisible, this "organ" weighs about two kilograms and comprises on the order of 1013 (10 trillion) cells of microorganisms.
According to molecular genetics research, the composition of species in gut flora is stable but can be altered dramatically due to changes in diet or antibiotic treatment. The community of microorganisms in the gut is a complex ecosystem encompassing hundreds of species whose genomes collectively encode 100 times more genetic information than the human genome. The aggregate of all genomes of gut microbiota known as the metagenome includes a "behavioral code" that determines trophic connections and other interactions within the gut community and with the host. The stability, or "health," of human gut microflora is essential for normal metabolism, cardiovascular health, food digestion and protection against infectious diseases.
During antibiotic treatment, the abundance of antibiotic resistance genes increases. When these genes are transmitted to a pathogen, this has dire consequences for both the individual patient and the society as a whole. An analysis of the functional composition of microbiota using metagenomic methods allows assessment of the relative abundance of the antibiotic resistance genes in human microbiota and thus predicts the capacity of an individual's microbiota to contribute to the onset of resistant pathogens. Vast volumes of metagenomes have been published, providing the opportunity to estimate variation of the resistome between different populations, as well as between patients with different diagnoses.
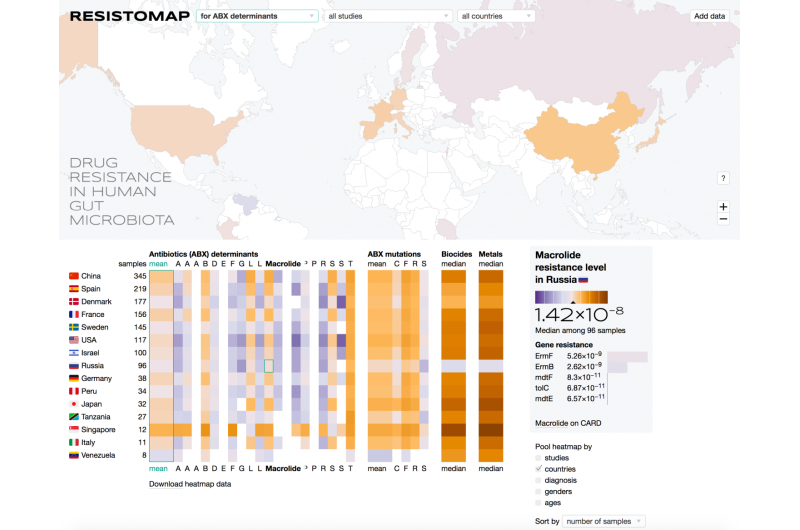
The ResistoMap has two main interactive work fields: a geographic map and a heat map. A user can choose the antibiotic group or country of interest to be displayed on the heat map and obtain a resistome cross section. The data can be filtered by the country of origin, gender, age and diagnosis. The current version of the interactive map developed by the authors draws on a dataset, which includes over 1,600 individuals from 12 studies covering 15 countries. However, the dataset can be expanded by additional input from users reflecting the findings of new published studies in a unified format.
Distinct national features
Using the ResistoMap, it is possible to estimate the global variation of the resistance to different groups of antibiotics and explore the associations between specific drugs and clinical factors or other metadata. For instance, the Danish gut metagenomes tend to demonstrate the lowest resistome among the European groups, whereas the French samples have the highest levels, particularly of the fluoroquinolones, a group of broad-spectrum anti-bacterial drugs. This is in agreement with the fact that France has the highest total antibiotic use across Western Europe, while the use of antimicrobial drugs in Denmark and Germany is moderate, both in health care and agriculture. At the opposite end of the spectrum, Chinese and Russian populations appear to have increased levels of resistome, which is likely due to looser regulation policies, frequent prescription of broad-spectrum antibiotics, and their over-the-counter availability without prescription. The lowest levels of microbiota resistome are observed in the Native population of Venezuela, which has no documented contacts with populations of developed countries. ResistoMap-informed analysis reveals certain novel trends that await further interpretation from the clinical standpoint.
Konstantin Yarygin, one of the creators of the visualization tool, says, "We anticipate that the exploratory analysis of global gut resistome enabled by the ResistoMap will provide new insights into how the use of antibiotics in medicine and agriculture could be optimized."
Medical experts offer a couple of rules everyone using antibiotics should follow to avoid losing ground in our ongoing war against microbes. The most important rule is that antibiotics should only be taken by prescription, in the dosage prescribed, and without interrupting the course (unless recommended by a doctor). According to Russian studies, one in four mothers does not complete the course of antibiotic treatment prescribed to her child. Exceeding the prescribed course duration is equally dangerous, as this means there is more time for the pathogens to develop resistance. It is thus necessary to take just enough antibiotics—and not too much—to treat an infection effectively. Narrow-spectrum antibiotics acting against specific types of bacteria are safer and should be given preference over their broad-spectrum counterparts. Provided that the infectious agent can be correctly identified, medications with a targeted effect make the survival of pathogenic bacteria less likely.
More information: Konstantin S. Yarygin et al, ResistoMap—online visualization of human gut microbiota antibiotic resistome, Bioinformatics (2017). DOI: 10.1093/bioinformatics/btx134



















