SPECT/CT combined with fluorescence imaging detects micrometastases
Researchers in The Netherlands have demonstrated that combining SPECT/CT and fluorescence imaging could help surgeons differentiate tumor tissue from normal tissue. The research is detailed in the featured basic science article of the May 2017 issue of The Journal of Nuclear Medicine.
The study focused on colorectal cancer (CRC) that metastasized beyond the primary tumor. CRC is the second most common cancer in men and the third most common in women. According to the American Cancer Society, more than 50,000 people in the U.S. are expected to die from the disease in 2017.
"This study shows that micrometastases of colorectal carcinoma can be detected specifically with fluorescence imaging and SPECT/CT before they become visible with the naked eye," says Marlène C.H. Hekman of the Department of Radiology and Nuclear Medicine at Radboudumc, Nijmegen, The Netherlands.
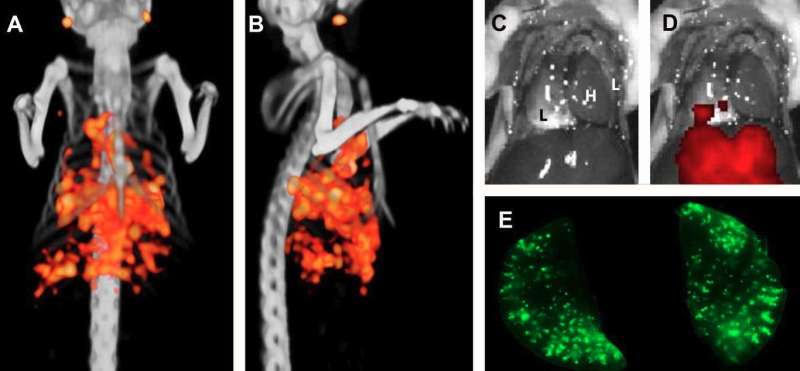
The researchers used a mouse model to show that pulmonary micrometastases of CRC can be identified with labetuzumab, labeled with both a near-infrared fluorescent dye (IRDye800CW) and a radioactive label (Indium-111). Labetuzumab, developed by Immunomedics, Inc., is an antibody that targets carcinoembryonic antigen (CEA), which is overexpressed in approximately 95 percent of CRC cases. Specifically, it is an investigational anti-CEA-related cell adhesion molecule 5 (CEACAM5) antibody.
Sub-millimeter pulmonary tumor colonies were visualized with both micro-SPECT and fluorescence imaging from the first week of tumor growth. In addition, the study demonstrated that dual-modality imaging can be used to guide resection of tumor lesions.
"Complete tumor resection is crucial for optimal prognosis of cancer patients," Hekman explains. "Intraoperative imaging can help the surgeon to resect residual disease completely. To be of optimal benefit in the operating room, dual-modality imaging should be able to detect very small tumor lesions that might otherwise be missed."
She points out, "The study shows that SPECT and fluorescence dual-modality imaging after injection of Indium-111-DTPA-labetuzumab-IRDye800CW is able to detect tiny CEA-expressing nodules. This strategy can also be used for other types of cancer, when a different tumor-targeting antibody is used. It is, therefore, relevant for a broad range of cancer types. Since our findings may be translated to a broad range of tumor types, dual-modality imaging may revolutionize oncological surgery and improve the prognosis of cancer patients."
More information: Marlène C.H. Hekman et al, Detection of Micrometastases Using SPECT/Fluorescence Dual-Modality Imaging in a CEA-Expressing Tumor Model, Journal of Nuclear Medicine (2017). DOI: 10.2967/jnumed.116.185470














