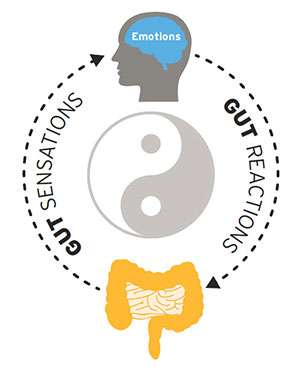
Understanding the constant dialogue that goes on between our gut and our brain

Just past midnight on Sept. 26, 1983, Lt. Colonel Stanislav Petrov, a member of the Soviet Air Defense Forces serving as the command-center duty officer for a nuclear early-warning system, faced a decision with unimaginable consequences.
Cold War tensions were running hot. The Soviet Union had recently shot down Korean Air Lines Flight 007, killing all 269 passengers and crew aboard the Boeing 747. The Soviets claimed the plane was on a spy mission and represented a deliberate provocation by the United States.
Now, in a bunker outside of Moscow where Petrov was stationed, alarm bells blared as Soviet satellites detected five U.S. ballistic missiles heading toward the USSR. Was this a real nuclear attack warranting retaliation? Or was it a false alarm? Gazing at a screen that flashed "launch" "launch" "launch," Petrov had only minutes to decide.
Thirty years later, Petrov reflected on his fateful decision to ignore the signal coming from the satellite detection system—which, of course, had turned out to be erroneous. But at the time, when he couldn't know that for sure, Petrov said he ultimately made the decision based on "a funny feeling in my gut."
In his book "The Mind-Gut Connection: How the Hidden Conversation Within Our Bodies Impacts Our Mood, Our Choices, and Our Overall Health" (Harper Collins, 2016), Dr. Emeran Mayer retells Petrov's story, and he notes how many historic and present-day decision-makers have cited unspecified feelings in their gut as tipping the balance on a difficult call.
To many of us, these "gut feelings" leading to "gut decisions" represent instincts with no basis in reasoned thought. But Dr. Mayer, professor of medicine, physiology and psychiatry and biobehavioral sciences and director of the UCLA Oppenheimer Center for Neurobiology of Stress and Resilience, has other ideas. Acting on his own inclinations developed as a medical student, he has spent the last 40 years building a scientific case for the inextricable link between the brain and the gut, often calling into question the conventional medical wisdom.
"The gut," Dr. Mayer says, "converses with the brain like no other organ. When people talk about going with their gut feelings on an important decision, what they're referring to is an intuitive knowledge based on the close relationship between our emotions and the sensations and feelings in the gastrointestinal (GI) tract."
These gut sensations go in both directions. "When you eat too much or have certain fatty foods, the changes in your gut can affect your mental state," Dr. Mayer notes. "And when you feel 'butterflies' or a rumbling in your stomach when you're nervous, or knots in your stomach when you're angry, your mental state is affecting your gut."
Dr. Mayer and the growing number of colleagues at UCLA and around the world who are interested in the mind-gut connection have been buoyed by the emerging evidence coming from studies of the gut microbiome—the 100-trillion-or-so bacteria and other microbes that make their home in our intestines. Research (mostly in the laboratory, but some in humans) suggests that emotions can affect the gut microbiota, and that, conversely, certain gut microbes can be mind-altering.
Yes, the gut has its essential roles to play in digestion and metabolism. But as Dr. Mayer suggested in an interview with Scientific American in 2010: "The system is way too complicated to have evolved only to make sure things move out of your colon."
Dr. Mayer is convinced that the brain-gut axis isn't a linear system, as it is often still viewed, but a circular-feedback loop operating through multiple communication channels. One of the most common channels is via activation of the vagus nerve, which extends from the gut lining to the brain stem. But interactions also can occur between the brain and the immune system (the gut hosts the majority of the body's immune cells) and between the brain and the endocrine system. When the communication channels go awry for one of a variety of reasons—including poor diet, stress or illness—the result can be physical-health problems such as digestive disorders and obesity or mental-health issues such as anxiety or depression. It's no coincidence, Dr. Mayer notes, that most patients with anxiety or depression also have abnormal gastrointestinal function.
Dr. Mayer's influence in shedding light on the mind-gut connection extends well beyond his own work; he has consulted with researchers looking at the relationship from a variety of vantage points. "Emeran has a unique ability to communicate across different levels of analysis—from the cellular to the physiological to the psychological to the behavioral," says Nancy Zucker, director of the Center for Eating Disorders at Duke University. "That enables researchers to better see the clinical and translational implications of our studies."
Zucker has sought Dr. Mayer's counsel on studies of the impact of gut-brain interactions on people with eating disorders and has collaborated with his group in studies of patients with anorexia nervosa. She is pursuing the hypothesis that a hypersensitivity to gut sensations fuels the disorder. "The widely accepted narrative is that these are individuals with a biological vulnerability, and the environment brings it out," Zucker says. "We believe that this vulnerability starts below the neck, and that it is neurological."
Well before the current "decade of the microbiome," Dr. Michael Gershon broke new ground with his book "The Second Brain" (Harper, 1998), referring to the collection of approximately 100 million neurons in the gut that constitute the enteric nervous system and act both independently and interdependently with the brain in our head. While it's no help in matters of philosophy, poetry and other forms of deep thought, Dr. Gershon noted, this second brain and how it interacts with the first one is a key factor in our physical and mental well-being.
The gut remains an underappreciated organ even by many scientists and physicians—perhaps because it isn't pleasant to look at or think about, suggests Dr. Gershon, who continues to serve as chairman of the Department of Anatomy and Cell Biology at Columbia University.
"What Emeran Mayer and others are finding is that there is a whole world of microorganisms that live in the gut," he says, "and that they are not just evil bacteria but are companions in life."
When Dr. Mayer was an M.D./Ph.D. student in the 1970s in Germany, he began to wonder if there was more to the brain-gut connection than was commonly believed. While participating in hospital rounds, he saw patients for whom extensive diagnostic testing had failed to reveal a cause of their chronic pain. Conditions characterized by chronic diarrhea, constipation, nausea and vomiting were common then and now, but rarely was the brain suspected as a factor under a prevailing view that the body consisted of independently operating parts. "I had always been very interested in psychology," Dr. Mayer says. "Seeing these patients further enhanced my interest in the possibility of a mind/body connection."
Finding a sponsor for such ideas wasn't easy. The resistance was such that Dr. Mayer initially had a hard time finding a laboratory and mentor for his dissertation, until finally he was taken in by a cardiovascular physiologist interested in the impact of mental stress on blood flow to the heart. Convinced by that experience that his theories could be studied scientifically, Dr. Mayer switched to the GI tract—and to the most obvious chronic disorder for his research, irritable bowel syndrome (IBS). An estimated one-in-seven people are believed to have IBS, which causes symptoms that can include abdominal pain, bloating, gas, constipation and diarrhea. Today, there is an evolving consensus that a brain-gut disorder is at play, but that was far from the mainstream opinion when Dr. Mayer was starting his career.

Over the next several decades, Dr. Mayer's research group became a leader in the use of brain imaging in human volunteer subjects to delineate the interactions between the mind and the gut in IBS and other brain-gut disorders (commonly referred to as functional gastrointestinal disorders), never losing sight of the big picture. "There are now more than 30 classified syndromes, and although the symptoms are different depending on what part of the gastrointestinal tract is affected by the dysregulation, the underlying mechanism is probably the same in all of them," Dr. Mayer says.
"Emeran's group was the first to use imaging to show that people with IBS are hyper-vigilant to the signaling coming from the gut, which makes them more susceptible to pain," says Yvette Taché, PhD, professor of medicine, co-director of the UCLA Oppenheimer Center for Neurobiology of Stress and Resilience and associate director of the CURE: Digestive Diseases Research Center at UCLA. "It was the first recognition that there was a brain component to this disease state."
Dr. Taché also has been a pioneer in unraveling brain-gut interactions in gastrointestinal disorders—in her case, through laboratory studies beginning in the 1980s that contributed to a new understanding of how stress can lead to gut dysfunction. Dr. Taché's group was the first to establish the importance of corticotropin-releasing factor in stress-related gut-function alterations. That finding was followed by the discovery of other peptides involved in transmitting information between the gut and the brain in a way that affects neurobehavioral and digestive functions.
"There wasn't even a descriptor for brain-gut interactions at the American Gastroenterology Association annual meeting when we were contributing those initial findings," Dr. Taché notes. "Now, it's widely recognized, and as the new kid on the block, the gut microbiome is taking this field of study to a new level."
DR. MAYER SPLITS HIS TIME BETWEEN RESEARCH AND A CLINICAL PRACTICE in which he has seen thousands of patients with various brain-gut disorders. He notes that emotions can have a profound effect on how the GI tract handles incoming food. "The setting of the table in your gut is different if you're angry vs. if you're happy vs. if you're anxious," he says.
For people whose brain-gut axis is chronically off-kilter, the problem extends both top-down and bottom-up. On the one hand, reactions to stress and emotions are supercharged. At the same time, these individuals are typically more sensitive to gut-generated signals, whether from food sensations or from feelings in their stomach and intestines. Dr. Mayer and his colleagues have found that the programming for this dysfunction occurs early in life. "We feel pretty strong, based on our clinical and research experience, that people who have a genetic predisposition, have been given antibiotics or have experienced adverse life events during their first few years, when the microbiome is being established and the brain is developing, are more vulnerable to the development of IBS symptoms under stress or following a GI infection later in life," Dr. Mayer says.
Even today, Dr. Mayer encounters resistance among other medical professionals to the notion that the mind and the gut are so interconnected. He believes this is driven, in part, by the way the healthcare system is structured. "I have patients referred to me who have undergone extensive repeated diagnostic evaluations with every possible technology, when what you really need to do is spend an hour talking with the patient to understand that it's most likely a brain-gut disorder, and we're better off trying integrative therapeutic interventions rather than wasting time and money on additional invasive procedures," he says.
Over the years, plenty of patients complaining of chronic pain that defies diagnosis have heard some variation of "it's in your head." As it turns out, the location wasn't off, even if there was a fundamental misunderstanding of the underpinnings. "A big portion of the pathophysiology is in the brain—but the proper focus should be on the mechanisms, not the psychology," Dr. Mayer says. "When you explain it to patients that way, they get it. It's not the same as hearing a frustrated gastroenterologist tell them, 'I've done all the tests and I think it's in your head.'"
Accordingly, mental-health professionals have an important—and underutilized—role to play in helping these patients. "We know from the imaging studies that there is a failure of the brain's cortico-limbical control mechanisms to restrain the stress-response and emotional-arousal systems, and cognitive behavioral therapy can retrain the prefrontal cortex to strengthen these inhibitory influences," Dr. Mayer says. "It's certainly not a miracle cure, but it has been shown in well-controlled studies to be superior to any medication that's currently available." Variants such as mindfulness-based stress reduction also have proven effective, says Dr. Mayer, with some imaging studies showing structural and functional changes in the brain as patients symptomatically improve.

EVEN AS HE WAS FOCUSED ON BRAIN-GUT DISORDERS SUCH AS IBS, Dr. Mayer always had an eye on the broader implications of brain-gut communications. The new frontier of microbiome research has fundamentally reset the brain-gut-research equation and shifted his attention to bigger-picture questions. With the aid of advanced mathematical modeling, systems biology and the most powerful tools of molecular biology, Dr. Mayer and investigators at the Oppenheimer Center are just beginning to understand the interactions between the body's two main regulatory organs—the gut microbiome and the central nervous system—and the implications for physical and mental health.
The study of gut microbiota has introduced a new dimension to scientists' understanding of the mind-gut link. "You could almost say the microbes sit at the interface between the brain and the gut, and anything that goes on in our brain will influence their behavior," Dr. Mayer says. "On the other hand, the microbes also respond to what we eat. So now we have to think about an integration of food-related metabolites and emotional- and stress-related behavior changes in microbes, resulting in a mix of metabolites and signaling molecules that in turn influence the nervous system." Now, for example, in addition to studying the brains of people with brain-gut disorders who undergo cognitive behavioral therapy, Dr. Mayer and his group are looking at whether or not the same individuals show a corresponding change in their gut microbiome.
"We have been cohabiting with these bacteria for hundreds of thousands of years, and we have developed a relationship we haven't even started to understand," observes Claudia Sanmiguel, MD (FEL '14), program director of the Ingestive Behavior and Obesity Program in the UCLA Vatche and Tamar Manoukian Division of Digestive Diseases. In that role, she studies the relation of brain-gut interactions in the development of obesity. Inspired by Dr. Mayer's imaging studies showing brain differences in GI disorders, Dr. Sanmiguel is conducting studies of patients both before and after weight-loss surgery in an effort to better understand the impact of changes in the gut microbiome on eating behaviors and the ability to lose weight. "We are seeing that the connections between changes in gut-microbiome metabolites and changes in the brain in obese people are quite significant," she says. "Our hope is that learning more about the type of gut microbiota and the related metabolites that are conducive to weight loss could lead to better nonsurgical treatments for obesity than the field has been able to develop up to this point."
While little has come out of gut-microbiome research in the way of therapies thus far, much intrigue surrounds the growing number of animal studies suggesting that manipulating the composition of bacteria in the gut could affect brain health and disease. "In animal models, we're seeing that changing the microbiome can produce substantial effects on their behavior, as well as differences in the structure and activity of brain cells," says Elaine Hsiao, PhD, assistant professor of medicine and integrative biology and physiology. "That is inspiring a great deal of effort to better understand what it is that bacteria or other microbes are doing to affect the brain and how they communicate with each other."
While at Caltech in 2013, Dr. Hsiao and her colleagues contributed to the intrigue with research showing that autism-like behavior could be produced in the offspring of mice they treated with a viral mimic during pregnancy. These offspring, which were found to have altered gut bacteria, showed reduced autism-like behaviors when treated with a health-promoting bacterium. Dr. Hsiao's UCLA lab continues to follow up on those findings with studies of the impact of microbiome changes on behaviors related to autism and other neurological disorders, including depression and epilepsy. "The promise in all of this research is that we are learning that microbes are part of normal human biology," Dr. Hsiao says. "Although we have a long way to go, the possibility of developing microbe-based therapeutics for mental and physiological disorders is exciting."
The same year that Dr. Hsiao and colleagues were attracting attention in the scientific community with their autism findings, Dr. Mayer and Kirsten Tillisch, MD '97 (RES '99, FEL '04), associate professor of medicine, made their own headlines with the first evidence that beneficial bacteria ingested in food could affect human brain function. In an early proof-of-concept study of healthy women, they found that those who regularly consumed probiotics through yogurt showed changes in the brain's responsiveness to an emotional attention task. Dr. Mayer remains skeptical that this will any time soon lead to certain diets being prescribed as primary brain therapy, but he believes a better understanding of the impact of the interactions between gut bacteria and the brain could lead to dietary and other interventions early in life—perhaps even during development in the womb—when the gut microbiome is under construction.
With the caveat that much more remains to be learned, Dr. Mayer does offer several practical recommendations in his book. These include getting in touch with one's gut feelings, engaging in mindfulness-based anxiety-reduction strategies and adopting a largely plant-based, whole-foods diet. He also advises steps for managing pre- and postnatal stress, along with early-childhood nutritional interventions to head off mind-gut-axis disorders and build/preserve microbiome diversity in children.
Dr. Mayer also offers a possible explanation for what might be the biological basis of gut-based decisions—those hard-to-pinpoint instincts we learn to trust. The Portugal-born neuroscientist Antonio Damasio, MD, has advanced the somatic-marker hypothesis, in which emotional experiences beginning early in life are associated with certain body responses that are stored in the brain as somatic markers. "Because the GI tract is so prominent, we know that the gut microbiome is a big part of encoding these experiences," Dr. Mayer says. "It may be that the brain acts like a supercomputer, with access to millions, or billions, of gut reactions that we've had from the day we were born, and draws from those experiences to tell us within milliseconds what decision is most likely to suit us."
This theory of instinctive decision-making will be difficult to prove, Dr. Mayer acknowledges. But his gut tells him it's the most likely candidate.

















