Cause of cancer form in the liver identified
In a new study, researchers from the University of Copenhagen have identified the two genes whose mutation cause a serious cancer form found in the liver. The result sets concrete goals for future treatment of the otherwise incurable disease.
There is no effective treatment for the cancer form found in the liver called fibrolamellar hepatocellular carcinoma, which is mainly found among children and young people. Operation of the tumour is the only treatment available, but after five years less than 40 per cent of the patients are alive. Therefore, it is vital to establish the cause of this form of cancer.
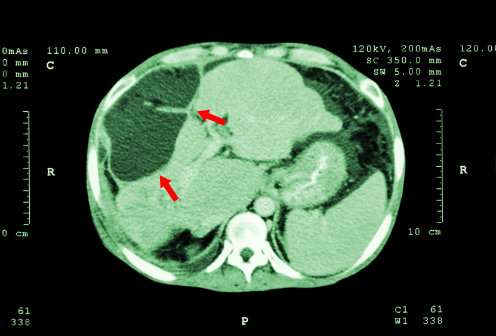
In a study published in the leading scientific journal Gastroenterology researchers from the University of Copenhagen have via tests on mice shown that the coupling of the two genes through a mutation causes a cancer tumour to develop in the liver. The researchers have made sure the genetic composition of the mutation in the mice is identical with the mutation found in human patients. This makes the researchers conclude that the gene mutation also leads to cancer in humans.
'We are now able to document that this mutation is the cause of this form of cancer. We suspected the mutation, but it is the first time it has been documented that it in fact does cause the disease. This makes it an obvious target for future treatment', says the author of the study, Associate Professor Morten Frödin from the Biotech Research & Innovation Centre, BRIC.
The researchers had suspected this mutation to be the cause of cancer, because a young, American student a couple of years ago sequenced the DNA in her own tumour and the tumour of other patients suffering from this fatal form of liver cancer. She discovered that all the patients suffering from the disease had the same mutation in their DNA.
Her results were published in the scientific journal of repute Science, and as a result of her work she met with then president Barack Obama. Her research also inspired the team of Danish researchers to examine whether the mutation in fact was the cause of cancer. To do so they performed tests on mice using a new method.
The researchers have used the revolutionary technology CRISPR/Cas9 that makes it possible to 'edit' our genetic material. They have produced CRISPR/Cas9 reagents, which would provoke precisely the desired fusion of the two genes. The reagents were injected into the mice's tails and then transported via the bloodstream to the liver. In the liver they created a mutation identical with the human mutation previously discovered by the American researcher.
Then the researchers were able to conclude that 12 or the 15 mice developed the expected type of tumour in the liver, while none of the 11 control mice did. According to the researchers, the result contains almost no 'noise', which may otherwise explain the development of cancer.
'The mice we used were "wild mice", in a scientific sense, which in practice means that they were completely normal. In other studies researchers deliberately damage the mice's liver to imitate a liver disease found among human patients or expose them to several different forms of mutations which may cause cancer. This was not necessary here. Because of our genetic design based on CRISPR/Cas9-technology we are certain that the main factor that can explain the cancer is the fusion of the two genes', Assistant Professor from BRIC and co-author of the study Francesco Niola explains.
Now the scene has been set for the development of drugs against the fusion gene as a treatment for this form of cancer. The researchers have a clear strategy for how this may be realised. They have already begun cooperating with a large pharmaceutical company.
More information: Lars H. Engelholm et al, CRISPR/Cas9 Engineering of Adult Mouse Liver Demonstrates That the Dnajb1 – Prkaca Gene Fusion is Sufficient to Induce Tumors Resembling Fibrolamellar Hepatocellular Carcinoma, Gastroenterology (2017). DOI: 10.1053/j.gastro.2017.09.008



















