Pushing the boundaries of melanoma border detection
Skin cancer experts will soon be able to benefit from a better way of spotting and identifying lesions, thanks to an improved image segmentation tool developed by computer scientists at Brunel University London.
Malignant melanoma is one of the most fatal forms of skin cancer, and has become more common – especially among white-skinned people exposed to the sun. In the UK, it is the fifth most common cancer, and since the early 1990s incidence rates have increased by 119%. Early detection of melanoma is essential to increase survival rates.
Getting a better picture
Working out the borders of melanoma lesions is an important step for dermatologists, who need an accurate way of reaching the correct clinical diagnosis, and to ensure the right area gets the right treatment.
But determining these boundaries can be a time-consuming, subjective and challenging task. Lesions have a large variation in size and colour, and the contrast between them and the surrounding healthy skin can be low – especially in early stages. Images of lesions are often further complicated by the presence of artefacts such as hair, reflections, oils and air bubbles.
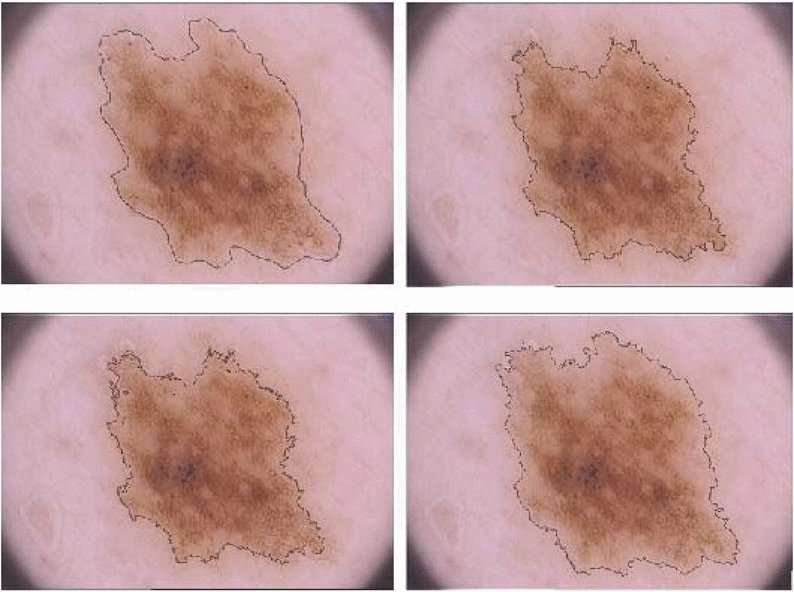
So dermatologists have long been helped by computers using image segmentation techniques to sort the pixels of lesion images into groups which share similar characteristics, such as texture, colour and shape.
Multi-dimensional modelling
Brunel's Khalid Eltayef, Yongmin Li and Xiaohui Liu have developed a fully automated, two-stage method for melanoma border detection which is more accurate than all previous techniques.
First, hair and other artefacts in the images are detected and removed using directional filters and image inpainting methods, which use information from the areas surrounding the artefacts.
Then the borders are delineated using a combination of two advanced, abstract methods.
In Particle Swarm Optimisation (PSO), candidate solutions for the whole image are modelled as a swarm of particles in multi-dimensional space – like scattering marbles over a model of a mountain range – and are tested and adjusted with mathematical functions until an overall global solution is recommended.
PSO has been used in other techniques, but has some drawbacks that are reduced by combining it with a Markov Random Field method, which optimises clusters of pixels and helps to minimise energy functions.
Enhanced accuracy
The Brunel team's method was tested on a standard set of 200 dermoscopic images, and the results were compared with seven leading alternative methods and the 'ground truth': the diagnoses reached by a dermatologist.
The proposed method achieved 95% accuracy, 94% sensitivity and 98% specificity – better than all the alternative methods, and so reducing the likelihood of false or missed diagnoses.
Mr Eltayef commented: "Our efficient and robust method can help dermatologists reach better diagnoses, and in a fast and accurate way. Once the code is loaded onto dermoscopy machines, the method will enhance these doctors' abilities – and therefore the outcomes of skin cancer patients."
More information: Khalid Eltayef et al, Lesion Segmentation in Dermoscopy Images Using Particle Swarm Optimization and Markov Random Field, 2017 IEEE 30th International Symposium on Computer-Based Medical Systems (CBMS) (2017). DOI: 10.1109/CBMS.2017.26
















