Why simple school sores often lead to heart and kidney disease in Indigenous children

Impetigo, also known as school sores, is a highly contagious bacterial skin infection that occurs in children far more frequently than adults. It is one of the most common bacterial infections in children aged two to five years. Impetigo happens when a break in the skin, from scratching an insect bite for instance, lets in disease-causing bacteria.
The bacteria responsible for impetigo are Staphylococcus aureus (S. aureus or staph) and Streptococcus pyogenes (S. pyogenes or group A strep). People with diabetes or other conditions that may affect the immune system, such as HIV infection, and those on medications that suppress immunity, are more susceptible.
While the infection itself is treatable, if left untreated it can lead to more serious conditions such as cellulitis (infection of the inner layers of skin) or abscess (painful collections of pus that build up under the skin). It can also progress to kidney disease, or it could cause acute rheumatic fever, which can affect the heart, joints, brain or skin.
Around 162 million children worldwide suffer from impetigo at any one time. They mostly live in resource-poor tropical countries or underprivileged populations in developed countries. In Australia, about 15,000 Indigenous children are estimated to suffer from impetigo – representing 40% of children in Indigenous communities.
Causes and symptoms
Impetigo can occur on top of other skin conditions, particularly itchy ones like eczema, scabies, insect bites, and head lice. Scratching the skin can break it and let the disease-causing bacteria in. A sore can be infectious for as long as it is weeping fluid, as the fluid and crusts of the sore contain infectious bacteria.
The time between becoming infected and developing symptoms is around four to ten days. Contact with the sore, or with things that have been in contact with the sore, can spread the infection to other people.
There are two forms of impetigo: non-bullous and bullous. Non-bullous, also known as the crusted form of impetigo, accounts for about 70% of all cases and can be caused by both S. aureus and S. pyogenes. It has a thick, soft, yellow crust below which is often a wet, red area.

Non-bullous impetigo spots grow slowly and are smaller than the fully grown spots of bullous, or blistering, impetigo. They are not usually painful but can be itchy. The lesions generally appear on the face and extremities, often at the location of already broken skin, such as an insect bite or eczema.
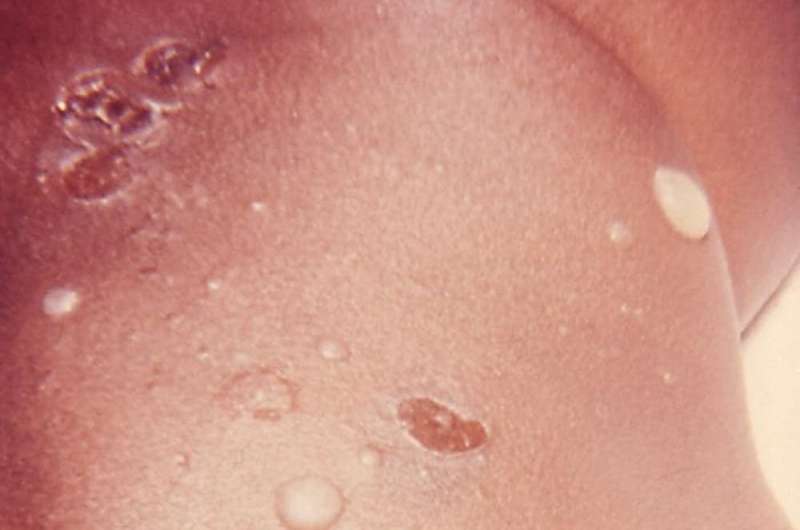
The bullous (blistering) form of impetigo is characterised by the formation of a large, fluid-filled irritating blister under the skin. It is caused exclusively by S. aureus and usually occurs where two skin surfaces touch or rub together, such as the armpits.
The blisters grow rapidly in size and number. They burst quickly and leave slightly wet or shiny areas with a brown crust at the edge. Those spots continue to grow quickly even after they break open and can be many centimetres wide. They are not usually painful but can be itchy.
What are the treatments?
As impetigo is highly contagious, good hygiene practices are essential for stopping the spread of infection. These include washing hands with soap, washing of infected clothes and towels, and covering the sore with a sticking plaster.
It's also recommended that the infected child be kept away from other children and school for 24 hours after starting treatment.
Impetigo is generally considered a mild disease that can resolve without treatment after a few weeks. But because it can cause more serious conditions, the child should be examined by a doctor and treated with appropriate antibiotics.
Topical antibiotics (creams) like mupirocin are recommended for mild forms of the infection. Oral antibiotics are used in more severe cases of impetigo, such as when multiple sores are present, or when topical treatments have been ineffective. The treatment should continue until all sores are completely healed. With treatment, symptoms are likely to be improved or cleared up after seven days.
What happens if it's not treated?
A possible consequence of untreated impetigo is an autoimmune kidney disease called acute post-streptococcal glomerulonephritis (APSGN). It's not frequently seen in developed countries but one estimate suggests that more than 390,000 children in less developed countries are affected, compared with about 13,000 children in more developed countries.
In Australia, data collected from 1991-2008 in the Northern Territory revealed that 95% of cases occurred in Indigenous Australians, with 98% of affected individuals living in remote locations. The average age was seven years old, with children younger than 15 accounting for 88% of all cases.
Given the association between APSGN and chronic kidney disease, it is important that predisposing skin infections are treated promptly and appropriately, and the risk of transmission or recurrences is minimised. Around 97% of deaths from APSGN occur in resource-poor countries or communities.
Acute rheumatic fever is another potential consequence of untreated impetigo. It is an autoimmune response to an untreated group A strep infection, and repeated episodes can damage the heart, leading to rheumatic heart disease.
Both rheumatic fever and rheumatic heart disease are preventable and generally not seen in industrialised countries. But rates of rheumatic fever and rheumatic heart diseases in Indigenous communities are up to 26 times those in non-Indigenous populations.
Between 1997 and 2013, 97% of patients diagnosed with acute rheumatic fever in the NT were Indigenous, despite Indigenous Australians representing about 30% of the NT population. Similarly, 94% of people diagnosed with rheumatic heart disease during this time were Indigenous, and Indigenous patients were younger than the non-Indigenous patients.
Poor hygiene, close living and lack of access to medical care are associated with impetigo and its related complications. Resources that help lessen these risk factors will also reduce the burden of impetigo and the diseases that can develop as a consequence.
This article was originally published on The Conversation. Read the original article.![]()

















