Higher doses of radiation don't improve survival in prostate cancer
A new study shows that higher doses of radiation do not improve survival for many patients with prostate cancer, compared with the standard radiation treatment. The analysis, which included 104 radiation therapy oncology groups across North America, was led by researchers at Washington University School of Medicine in St. Louis.
Past studies have shown that gradually escalating the radiation dose resulted in improved cancer control, such as slower tumor growth and lower levels of prostate-specific antigen (PSA), an indicator of cancer growth. The new study, published March 15 in JAMA Oncology, is the first that is large enough to examine whether these improved measurements translate into longer survival for patients.
"Our goal is to improve survival, but we didn't see that despite advances in modern radiotherapy," said first author Jeff M. Michalski, MD, the Carlos A. Perez Distinguished Professor of Radiation Oncology. "But we did see significantly lower rates of recurrence, tumor growth and metastatic disease—tumors that spread—in the group that received the higher radiation dose. Still, that didn't translate into better survival. The patients in the trial did better than we anticipated, and part of that may have been because of improvements in metastatic cancer therapy over the 10 years of the trial."
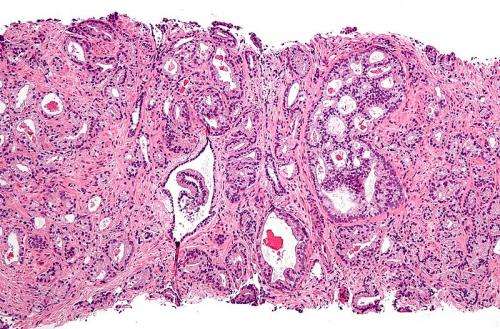
The study included about 1,500 patients with intermediate-risk prostate cancer, the risk category in which most patients fall. To be classified in this risk category, patients generally have PSA scores of 10-20 ng/ml and a Gleason score of seven, the latter of which is a measure of tumor aggressiveness. Both treatment groups received external beam radiation. The standard group received a radiation dose of 70.2 gray delivered over 39 treatment visits. The investigational group received increasing doses up to 79.2 gray delivered over 44 visits. (A gray is the standard measure of radiation a material has absorbed.)
Of the 748 men receiving standard treatment, 75 percent were still alive after eight years of follow-up. Of the 751 men receiving the dose-escalation treatment, 76 percent were alive at the eight-year mark—a difference that is not statistically significant. These overall survival rates include deaths for any cause, not just those due to prostate cancer. Over the course of the study, 51 patients died of prostate cancer, which is 3.4 percent of all patients enrolled. At the eight-year mark, the death rate due to prostate cancer for patients receiving standard treatment was 4 percent compared with 2 percent for patients receiving the escalating dose. These rates also were not statistically different.
While there was no difference in overall survival numbers, Michalski pointed out some differences in side effects and in whether further treatment was needed later. Such differences could help doctors and patients in deciding the best treatment course.
Patients in the standard dose group were more likely to undergo further therapies to control tumors that had grown larger or that had spread to another site in the body. But patients in the escalating dose group experienced more side effects—such as urinary irritation or rectal bleeding—sometimes years after treatment.
During the 10 years it took to enroll enough patients in the trial, Michalski said, at least six new therapies were approved for recurrent or metastatic prostate cancer, and these therapies have been shown to improve survival. It is possible the patients in the standard treatment arm—who were shown to need more follow-up therapies—would not have done as well as the group receiving the escalating dose had these new therapies not become available.
"If there is a difference between standard and escalating doses, it's hard to show it when the patients who later develop recurrent cancer can have their lives extended through the use of additional therapies," said Michalski, who treats patients at Siteman Cancer Center at Washington University School of Medicine and Barnes-Jewish Hospital. "Of course, these additional therapies have their own side effects, as does the higher initial dose of radiation therapy. In addition, the selective use of androgen withdrawal therapy has been shown to improve survival in men treated with radiation therapy. This treatment can be combined with either standard or higher dose radiation therapy."
"If we can safely deliver the higher dose of radiation, my opinion is to do that," Michalski added. "It does show lower risk of recurrence, which results in better quality of life. But if we can't achieve those 'safe' radiation dose goals, we shouldn't put the patient at risk of serious side effects down the line by giving the higher dose. If we can't spare the rectum or the bladder well enough, for example, we should probably back off the radiation dose. It's important to develop treatment plans for each patient on a case-by-case basis."
More information: Michalski JM, Moughan J, Purdy J, Bosch W, Bruner DW, Bahary JP, Lau H, Duclos M, Parliament M, Morton G, Hamstra D, Seider M, Lock MI, Patel M, Gay H, Vigneault E, Winter K, Sandler H. Effect of standard vs. dose-escalated radiation therapy for patients with intermediate-risk prostate cancer: The NRG Oncology RTOG 0126 randomized clinical trial. JAMA Oncology. March 15, 2018.













