Smartphone-assisted neuroendoscopy
Smartphones have changed the ways in which we live. They connect us with friends and families by phone, texts, and pictures. They warn us about what weather to expect and what traffic patterns we'll face on our way to work. They keep us abreast of all the news of the day and in touch with colleagues and clients.
Here's another item we can add to the list: smartphones can assist neurosurgeons in performing intricate surgeries. In a paper published today in the Journal of Neurosurgery, "Smartphone-assisted minimally invasive neurosurgery," Mauricio Mandel, MD, and colleagues from São Paulo, Brazil, describe a smartphone-endoscope device for use in minimally invasive neurosurgery. These authors found the device easy to use, efficient, cost effective, and a great learning tool for less experienced neurosurgeons.
Background
Neuroendoscopy is a minimally invasive neurosurgical procedure performed in select cases to correct hydrocephalus, remove tumors, treat vascular disease, and manage other disorders. Neuroendoscopic procedures generally result in less pain, shorter recovery times, and less scarring than craniotomy (open surgery).
During the neuroendoscopic procedure, a rigid or flexible neuroendoscope is inserted through a small incision in the skull, nose, or roof of the mouth and moved on to the planned surgical site in the brain, ventricles, or subdural or subarachnoid spaces. The neuroendoscope contains a light source to illuminate the surgical field, a lens for magnification, and a camera, which sends images to a nearby video monitor so that surgeons can see where they are operating. The neuroendoscope also contains channels and ports through which surgeons can insert and maneuver endoscopic instruments and irrigate the surgical site.
Present Study
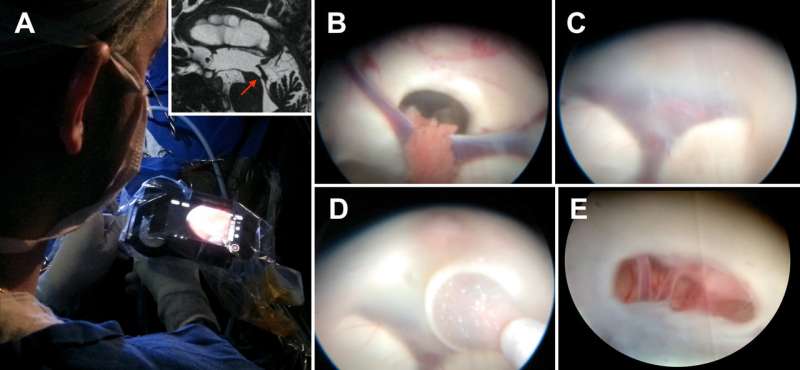
In this paper, the authors describe their experiences in performing a variety of neurosurgical procedures with the aid of smartphone-endoscope integration: intraventricular procedures, such as treatment for hydrocephalus; vascular neurosurgery, such as aneurysm clipping or cavernoma resection; and emergency neurosurgery, such as evacuation of a subdural or intracranial hematoma. The authors demonstrate how a smartphone takes the place of the video camera usually used in neuroendoscopy and makes the presence of a separate video monitor optional.
During minimally invasive surgeries performed in 42 patients, a fully charged smartphone (iPhone models 4, 5, and 6) was attached to the front of the neuroendoscope by means of an adapter. The primary surgeon focused directly on the iPhone screen in front of him or her, rather than off to one side where the video monitor normally stands. The smartphone relayed images from the screen via Wi-Fi to a video monitor placed elsewhere in the operating room.
The video monitor remained in the operating room so that other members of the surgical team could view the procedure or in case the primary surgeon wished to revert to more conventional neuroendoscopy. The surgeons who tested the smartphone-endoscope device found images provided by the smartphone to be sufficient and did not switch to the conventional method.
In each case the device worked well. All surgeries were successful, and no complications related to use of the smartphone occurred.
Based on their experience, the authors list several advantages of using smartphone-assisted neuroendoscopy:
- The smartphone is light-weight and small. It attaches easily to the endoscope by means of an adapter.
- Despite the small size of the smartphone screen, its high-definition image provides an excellent view of the surgical site.
- The smartphone camera supports real-time video acquisition, storage, and transmission via a variety of wireless technologies (Wi-Fi, 4G, Bluetooth, etc.). Images viewed by the primary surgeon can be simultaneously shared with the rest of the operative team on a video monitor, streamed directly to other colleagues or websites, and recorded for review and teaching purposes.
- Images can be manipulated in real time using camera functions on the smartphone.
- Compared with standard video equipment, smartphones are cheaper, more portable, and do not require an external power source. Should the battery become depleted during a prolonged surgery, the smartphone can be recharged without an interruption in the procedure.
- Having the smartphone screen directly in front of the primary surgeon allows "a more dynamic and intuitive approach to resection" than can be experienced when a surgeon has to look away from the endoscope being manipulated to view the surgical field on a separate video monitor.
- The learning curve for neurosurgical residents less experienced in neuroendoscopy is reduced when the smartphone is used.
The authors recognize that their study is preliminary and the number of cases is low. Nevertheless, they suggest that the smartphone-endoscope device may provide an alternative method of performing neuroendoscopy. The relatively inexpensive costs of a smartphone and adapter could prove beneficial in underserved areas and in countries whose medical infrastructure cannot support expensive equipment.
When asked about the study, Dr. Mandel said, "The most interesting aspect of this project was that our initial goal was to reduce the cost of the neuroendoscopic video set, but, in the end, we came across a new, more intuitive and fluid method of performing these procedures."
More information: Mandel M, Petito CE, Tutihashi R, Paiva W, Abramovicz Mandel S, Pinto FCG, Ferreira de Andrade A, Teixeira MJ, Figueiredo EG . Smartphone-assisted minimally invasive neurosurgery. Journal of Neurosurgery, published online, ahead of print, March 13, 2018; DOI: 10.3171/2017.6.JNS1712




















