Researchers develop new technology to manage cancer pain
As cancer patients become increasingly ill toward the end of their lives, their pain often intensifies and increases in frequency. This is distressing not only to the patient, but also to the patient's caregivers, often a spouse or partner.
Effectively managing that pain with medications and other therapies is of utmost importance, but also difficult to accomplish for most lay caregivers.
"Pain care can become a vicious cycle; as the patient experiences more pain, the caregiver becomes increasingly stressed, which often affects the patient's sense of well-being," said Virginia LeBaron, a University of Virginia nursing professor and cancer care researcher. "As both the patient and home caregiver experience increased anxiety, they can both lose sleep and the stress and anxiety further intensify, which can affect treatment adherence."
To help alleviate these reciprocal symptoms of cancer pain, LeBaron is working with two other UVA researchers, an engineer and a physician, plus graduate engineering and nursing students, on a pilot research project using in-home wireless sensing technology to help patients and lay caregivers better manage cancer pain in the home setting.
"At a time when the nation faces an opioid addiction crisis, we are looking for ways to ensure the safe use of prescription opioid medications, while also keeping patients comfortable and engaged," LeBaron said. "We want to help caregivers and patients find that balance where they can safely relieve the pain symptoms of advanced cancer and maintain the highest quality of life possible."
The UVA research team, made up of LeBaron; John Lach, an electrical and computer engineering professor; and Dr. Leslie Blackhall, a palliative care physician, is developing and deploying an innovative, in-home system of wireless sensing technology that records factors that may contribute to increased pain. The goal is to better understand and ultimately predict the triggers and circumstances – such as stress, sleeplessness and various activities – that can worsen pain at different times of the day and night.
The research is necessary, the researchers say, because little is known about pain management outside of clinical and professional settings such as hospitals, nursing homes and hospice care. Doctors prescribe painkillers based on the type of disease, its stage, and how much pain the patient says he or she is experiencing, often on a zero-to-10 severity scale.
But pain levels and frequency fluctuate over time and under different conditions, and pain is exacerbated by anxiety and sleeplessness, the time of day or night, whether visitors or present or not, and many other factors. For this reason, pain management in the home, in real time, can be very different from pain management at a clinic during a relatively short visit.
"We want to understand pain and pain care dynamics, as it happens," said Lach, who developed the wireless sensing technology at his UVA lab. "And we want to provide support to caregivers as they try to manage the pain experienced by the patients they support. We hope to identify the factors that can cause pain to escalate, before it happens, so that that pain can be mitigated in advance."
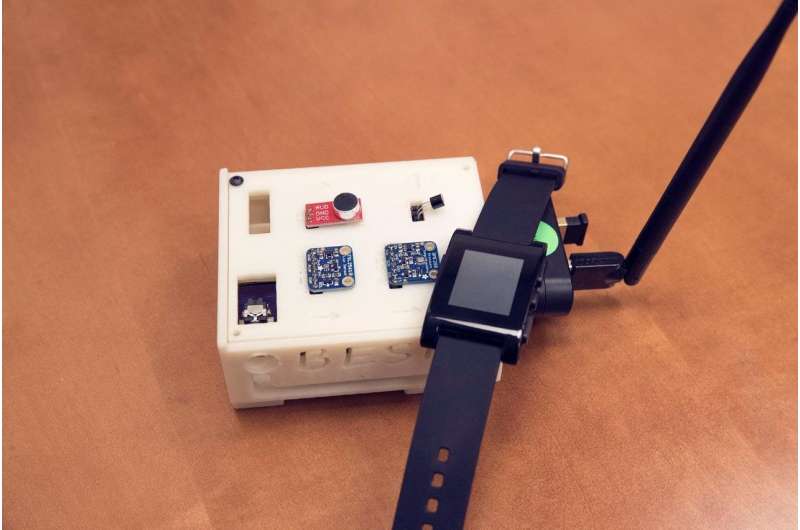
The technology consists of two primary devices: a wristwatch-like device that continuously measures physiological activities and responses, such as heart rate, body temperature and motion; and room sensors that record conditions and activities in the home that may influence pain, such as temperature changes, light levels, visitor activity and noise that can cause stress and interfere with rest.
The researchers also will conduct brief electronic surveys with study participants to seek correlations regarding their reported pain levels and the data recorded by the sensors. The technology, if it works as anticipated, would be of particular value to people in rural areas and small towns who do not have ready access to clinical care and home nurses. It could also be of help to hospice caregivers.
"The idea is that a better understanding of the factors and patterns that can affect pain intensity and frequency will help us identify effective and customized pain-management strategies by the caregiver for the patient," Lach said. "This could reduce the stress of both the caregiver and the patient."
According to LeBaron, reduced stress can also reduce pain, as pain and stress are closely connected.
"It would be great if we can monitor and detect pain before it escalates, so the caregiver can receive a warning and then give appropriate care at the right time," LeBaron said. "Being proactive, rather than reactive, would go a long way toward alleviating patient and caregiver distress."


















