Older melanoma patients have better response to immune checkpoint blockade therapy
Patient age correlates with response to immunotherapy in melanoma and depleting regulatory T cells in young patients may have a therapeutic potential to enhance response in younger patients, according to research from The Wistar Institute. Study results were published online in Clinical Cancer Research.
Immune checkpoint blockade therapy has been recently approved for treatment of melanoma based on its ability to produce durable disease control. Not all patients benefit from this therapeutic approach and some responders eventually develop resistance, highlighting the need for biomarkers that could help predict patient benefit and guide therapeutic choices.
"We have shown that the characteristics of the aged tumor microenvironment in older patients promote resistance to melanoma targeted therapies, highlighting the importance of considering patient age when predicting response to therapy," said Ashani Weeraratna, Ph.D., Ira Brind Associate Professor and co-program leader of the Immunology, Microenvironment and Metastasis Program at Wistar and corresponding author of the paper.
Based on this consideration, Weeraratna and collaborators set to analyze the impact of age on response to immunotherapy. "We were initially surprised to find that older patients fare better on immune checkpoint blockade therapy," she added.
The researchers analyzed a multi-national, multi-institutional cohort of almost 500 melanoma patients treated with pembrolizumab, an anti-programmed cell death receptor-1 (PD1) checkpoint therapy. They observed a significant difference in response to treatment by age, specifically that older patients had a decreased chance of disease progression after therapy, irrespective of gender and prior treatment with targeted therapies.
This observation was confirmed in mouse models of melanoma. In fact, genetically identical tumors responded more to anti-PD1 treatment when transplanted in old mice than in young mice, suggesting that the difference is ascribable to the environment in which the tumor develops.
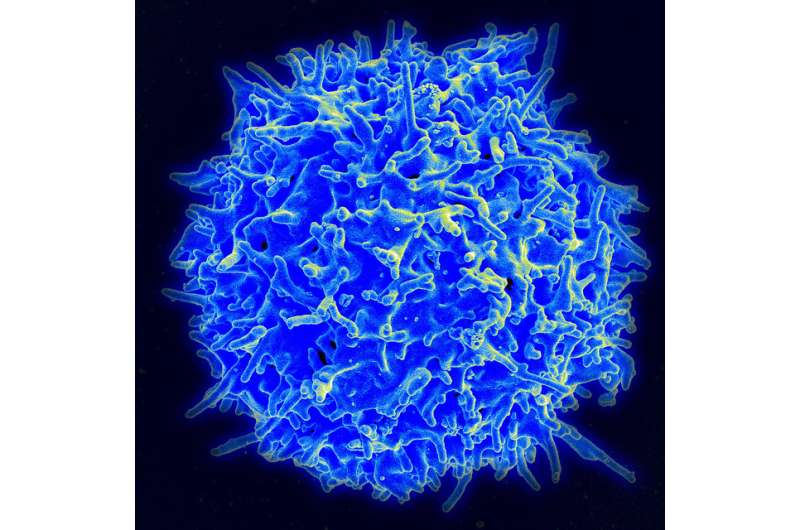
The researchers analyzed the immune cell composition of the old and young tumor microenvironment both in patient-derived tissues and in mouse models and found a significant decrease in tumor infiltration of regulatory T cells (Treg) with age. These cells, characterized by expression of the FOXP3 marker, suppress the anti-tumor immune response and reduce response to anticancer immunotherapy. In parallel with a decrease in the percentage of Treg cells, older age correlated with increased presence of killer CD8 T cells, which are the primary effectors in the response to immune checkpoint blockade therapy.
Based on these observations, the researchers depleted Treg cells in the young mouse model by targeting them with an antibody against CD25, which is predominantly expressed at high levels on Treg cells. Combining anti-PD1 and anti-CD25 treatment was significantly more effective than anti-PD1 alone and they obtained response rates similar to those seen in aged mice, suggesting that overcoming the immune suppression observed in the young microenvironment helps to restore sensitivity to immunotherapy.
"Our study shows that age is an important factor to consider when administering immunotherapy to melanoma patients," added Weeraratna. "A combination approach to deplete immune suppressive cells in combination with checkpoint blockade therapy might benefit younger patients, although further studies will be required to evaluate more broadly the potential immune toxicities of this approach."
More information: Curtis H. Kugel et al, Age Correlates with Response to Anti-PD1, Reflecting Age-Related Differences in Intratumoral Effector and Regulatory T-Cell Populations, Clinical Cancer Research (2018). dx.doi.org/10.1158/1078-0432.CCR-18-1116
















