No substantial benefit from transplantation reported for a high-risk leukemia subtype
Checking for minimal residual disease early in treatment can help some young high-risk leukemia patients avoid bone marrow transplantation without compromising their long-term survival A St. Jude Children's Research Hospital investigator led the international retrospective analysis that appears today in the Journal of Clinical Oncology.
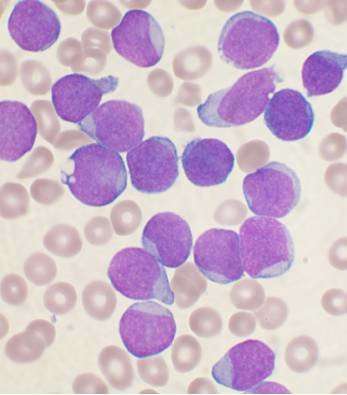
The study involved children and adolescents with hypodiploid acute lymphoblastic leukemia (ALL). This high-risk subtype accounts for about 2 percent of pediatric ALL cases. It is characterized by a poor prognosis and leukemic cells with 25 to 44 chromosomes rather than the usual 46.
The historically poor prognosis has prompted many leukemia specialists to advocate for treating these patients with intensive chemotherapy followed by allogeneic bone marrow transplantation. Transplantation, however, carries its own short- and long-term health risks.
The largest study yet of children and adolescents with hypodiploid ALL found that transplantation did not significantly improve survival compared to chemotherapy alone. However, contemporary risk-directed therapy—with dose intensity based on early treatment response determined by measuring minimal residual disease levels in bone marrow following remission induction chemotherapy—was more closely associated with better patient outcomes.
Response and survival
"This study confirms our earlier observation that patients with hypodiploid ALL who have no evidence of minimal residual disease after remission induction therapy should not be transplanted," said first and corresponding author Ching-Hon Pui, M.D., chair of the St. Jude Department of Oncology. "We recommend continued treatment with intensive chemotherapy."
Remission induction therapy encompasses the first four to six weeks of chemotherapy. Minimal residual disease (MRD) negative patients are defined as having fewer than 1 leukemic cell in 10,000 white blood cells in bone marrow.
Overall, 58 percent of patients in the study became long-term survivors. Disease-free, long-term survival rates were 75 percent for the 87 patients who were MRD negative after remission-induction chemotherapy. Survival rates were similar, 74 percent, for hypodiploid patients with 44 rather than fewer chromosomes.
Transplantation and survival
The study included data from 306 hypodiploid ALL patients who were enrolled on 16 different protocols of national study groups or major institutions between 1997 and 2013.
Questions remain about how to improve outcomes for patients with fewer than 44 chromosomes with minimal residual disease following induction therapy.
This analysis found that compared to intensive chemotherapy alone, transplantation did not provide a significant survival advantage for patients with fewer than 44 chromosomes. Adjusted five-year overall survival was 57.7 percent for the 186 patients treated with chemotherapy alone versus 68.9 percent for the 42 patients treated with both chemotherapy and bone marrow transplantation. Pui said the difference was not significant, particularly considering the long-term health risks, including second cancers, associated with transplant-related radiation. He said additional studies are warranted for treating hypodiploid ALL with immuno- or cellular therapies, which do not involve radiation.
Precision medicine
Researchers said the growth of precision medicines holds promise for improved outcomes for patients with hypodiploid ALL and other high-risk subtypes. The list of promising possible treatments includes chimeric antigen receptor-modified T cells, genetically modified antibodies and inhibitors targeting cell signaling pathways that drive proliferation.
The study included 17 co-authors from 17 medical centers and research institutions in Europe, Asia and Israel.
The research was funded in part by grants (CA21765, CA36401, CA176063, GM92666) from the National Institutes of Health, and ALSAC, the fundraising and awareness organization of St. Jude.

















