New method for monitoring residual disease after treatment in children with neuroblastoma
A research group led by Professor NISHIMURA Noriyuki (Graduate School of Health Sciences, Kobe University) has developed a new method to monitor the residual disease after treatment in high-risk neuroblastoma patients. The method could be utilized to evaluate treatment response and facilitate early diagnosis of tumor relapse/regrowth.
This monitoring method was developed by a group consisting of Assistant Professor YAMAMOTO Nobuyuki and Project Assistant Professor UEMURA Suguru (both of the Graduate School of Medicine, Kobe University), and from Hyogo Prefectural Kobe Children's Hospital; Vice Director Dr. KOSAKA Yoshiyuki, Department Head Dr. HASEGAWA Daiichiro and chief physician Dr. ISHIDA Toshiaki. Research collaboration and support was also provided by SYSMEX.
These results were first published in the Journal of Molecular Diagnostics on December 11, 2019.
Neuroblastoma is a type of cancer that affects children. It is characterized by solid tumors that develop from immature nerve cells in the sympathetic nervous system, commonly in and around the adrenal glands. Over 50% of patients with high-risk neuroblastoma experience tumor relapse or regrowth and their long term survival rate is as low as 40%. Eliminating MRD is vital to sustain treatment effectiveness and improve patient prognosis, and various monitoring methods have been utilized.
Monitoring methods up until now have evaluated MRD using real-time PCR (qPCR). This monitoring has involved measuring the levels of various neuroblastoma-associated markers, high levels of which indicate the development of neuroblastoma cells across cancerous and non-cancerous stem cells.
The current study sought to more accurately evaluate these pathological changes. Out of the neuroblastoma-associated markers that are highly expressed in neuroblastoma cells, the research group selected seven markers that are particularly abundant in the cancer stem cells that cause tumor relapse/regrowth. To detect the levels of these seven markers, the research group used droplet digital PCR (ddPCR), which provides a more sensitive and reproducible way of measuring these markers in a sample than qPCR.
This research team previously developed a qPCR-based system that was used to detect levels of eleven markers associated with the cancer stem cells that cause neuroblastoma reoccurrence. This method enabled them to monitor MRD in high-risk neuroblastoma patients. However, it was difficult to accurately track the changes taking place using qPCR. For the current study, the research group decided to use the more sensitive and reproducible ddPCR to evaluate MRD.
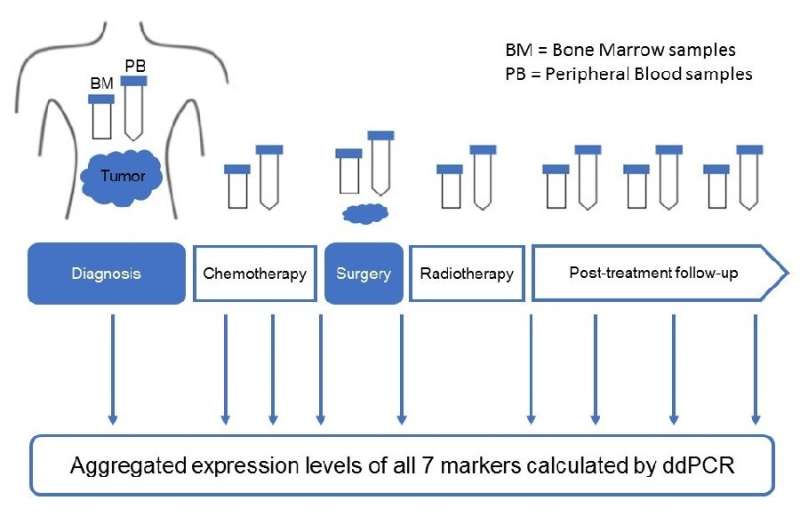
First of all, 208 bone marrow samples and 67 peripheral blood samples were taken from high- risk neuroblastoma patients, and 103 bone marrow samples and 107 peripheral blood samples were obtained from healthy individuals (control). Seven markers were selected from among the eleven markers that are highly expressed in the cancer stem cells that cause neuroblastoma regrowth/relapse. Using ddPCR, they calculated the levels of these seven markers in the bone marrow and peripheral blood samples.
The research group discovered that they could more accurately diagnose high-risk neuroblastoma patients when calculating the aggregated expression levels of all seven markers using ddPCR, as opposed to looking at the expression level of each marker individually. The changes in the expression levels of these seven markers reflected the amount of tumors, the stage of illness (remission, stable, or progression) and the sample collection period (diagnosis, treatment, post-treatment, or relapse).
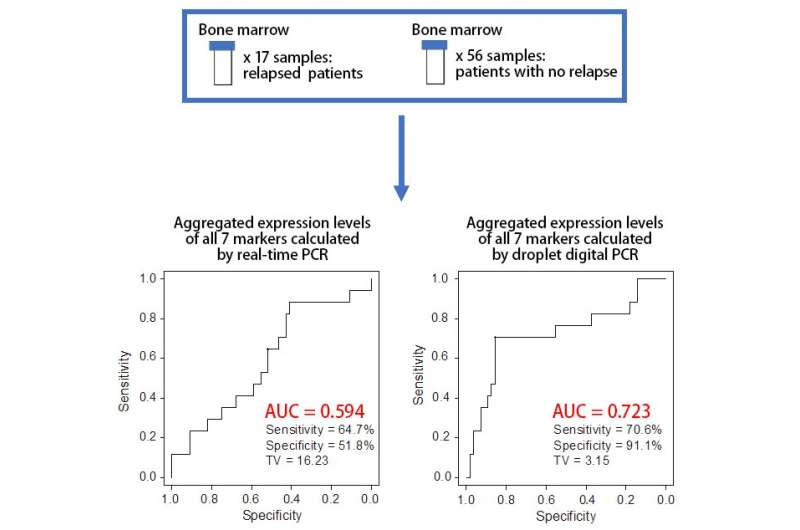
The expression levels of the seven markers were calculated for 73 bone marrow samples obtained from post-treatment high-risk neuroblastoma patients. The expression levels of the markers in the bone marrow samples of the 17 patients who had suffered tumor relapse/regrowth was significantly higher compared to the levels in the 56 patients who hadn't. By comparing the two PCR methods using the same 73 samples, it was predicted that the expression levels of the seven markers calculated by ddPCR would be able to more accurately predict tumor relapse/regrowth than qPCR.
Based on these results, it is expected that the ddPCR monitoring method developed by this study will improve the monitoring of MRD in high-risk neuroblastoma patients, enabling the possibility of tumor relapse or regrowth to be more accurately predicted.
The results of this research suggest that it is possible to accurately monitor MRD in post-treatment high-risk neuroblastoma patients. Next, this methodology needs to be evaluated through prospective clinical studies on a larger number of patients across multiple hospitals. It is expected that this monitoring method can be used as a basis for predicting patients' prognoses and developing new treatments for high-risk neuroblastoma patients.
More information: Khin K.M. Thwin et al. Level of Seven Neuroblastoma-Associated mRNAs Detected by Droplet Digital PCR Is Associated with Tumor Relapse/Regrowth of High-Risk Neuroblastoma Patients, The Journal of Molecular Diagnostics (2019). DOI: 10.1016/j.jmoldx.2019.10.012



















