Effective vaccine, efficient production processes necessary for mass immunization
Even though there still isn't a vaccine against the coronavirus, researchers and policymakers are already discussing which groups should be protected first. But one thing is clear: As soon as a vaccine is found, it must be produced quickly and in large quantities. Only then will it be possible to contain the COVID-19 pandemic without the current restrictions on social life. Biotechnical processes to produce viruses developed by scientists at the Max Planck Institute for Dynamics of Complex Technical Systems in Magdeburg could help. The team from Magdeburg now wants to adapt these methods to the production of a corona vaccine. The researchers from Magdeburg are interested not only in the large-scale production of viruses and their efficient purification for use as a vaccine, but also in the search for suitable immunogens against COVID-19.
The race for a vaccination against the coronavirus SARS-CoV-2 will take place in two stages. Scientists around the world are diligently searching for a vaccine that will effectively mobilize the human immune system against the COVID-19 pathogen. However, vaccine development will be only an intermediate success. They will then need to produce large quantities of a highly purified vaccine, and do it very quickly. Udo Reichl, Director at the Max Planck Institute for Complex Technical Systems in Magdeburg, and his colleagues are involved in both stages of the race to achieve the broadest possible immunization of the world population.
Different routes to a corona vaccine
In the search for a vaccine, researchers are currently pursuing different approaches. "At present, the most promising approach is probably to incorporate antigens such as the spike S1 protein of the coronavirus, for example, into the MVA virus and thus present it to the human immune system," says Reichl.
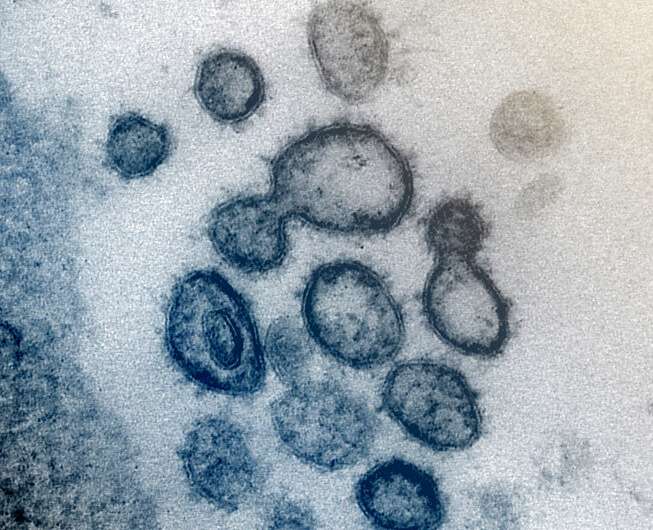
The MVA (modified vaccinia Ankara) virus is a harmless virus often used to display proteins from pathogens to the human immune system. Researchers are also testing individual components of the virus such as parts of its genetic blueprint or recombinant proteins as immunogens (i.e., as trainers for the human immune system). In the latter case, many groups are concentrating on the spike S1 protein, which gives the coronaviruses their name because of the characteristic projections that appear like the peaks of a crown.
Other groups are studying live attenuated or inactivated viruses. Vaccine manufacturers would like to avoid the variant of an inactivated virus because this would entail producing actual SARS-CoV-2, which is associated with high safety requirements. However, they may not be able to get around it. For example, the Chinese company Sinovac has just presented the results of its first successful tests with inactivated SARS-CoV-2. "This may be the way to get the best vaccine," says Reichl.
Animal cells as factories for viruses
Viruses and viral vectors, which, like MVA, serve as transporters of pathogen proteins, must be produced in large quantities for vaccine production. Among other things, animal cells can serve as factories. However, these must first be cultured in large numbers. This is the special field of Udo Reichl and Yvonne Genzel, who heads a research group in his Department. The two scientists have developed processes with which the cells of monkeys, hamsters, dogs, or birds can be propagated very efficiently. An important aspect is that the cells are continuously supplied with a fresh nutrient solution and waste products are quickly removed.
"In our processes, we can produce up to 10 or 100 million cells per millilitre," says Reichl. The researchers have already produced influenza, Zika and yellow fever viruses in animal cell suspensions. In some cases, they were able to obtain several billion viruses per millilitre. In the turbo-culture of animal cells, MVA viruses can also be produced on a large scale. The processes could also enable the Magdeburg team to produce the SARS-CoV-2 viruses in large quantities if they prove to be the best immunogen against COVID-19 in either attenuated or inactivated form.
In addition to suspension cells, adherent cells that require a surface for growth are also suitable for the production of coronaviruses. Vero cells, comprising a cell line from an African green monkey, are one such example. Sinovac used this cell line to generate the coronaviruses for its study. Udo Reichl and his team have also designed efficient processes for the culture of Vero cells. The researchers are currently preparing studies to test these methods in the production of coronaviruses, but it is highly challenging. "Because we will be working with highly infectious material, we urgently need an S3 laboratory with negative pressure and double-door systems," says Reichl. There is currently no such a high security laboratory at his institute. He is therefore planning this project together with Judith Gottwein from the University of Copenhagen, which has an S3 laboratory.
A purification method for vaccination viruses with cellulose and polyethylene glycol
If coronaviruses or viral vectors prove to be the most effective immunogens, the mass production of these will not be enough to achieve an effective and readily available vaccine. In order to produce such a vaccine, it must be possible to purify virus particles at a high yield. The Magdeburg team is also focusing on this step. The researchers have developed a process that enables them to achieve a yield of around 95% after purification of a virus from the production medium. They use a special form of chromatography that involves cellulose carriers and polyethylene glycol (PEG). With this method, PEG is added to the virus-containing liquid, which is then passed through several membranes. The high PEG content causes the viruses to attach themselves to the cellulose surface. The impurities, on the other hand, flow straight through the membranes. The researchers then rinse the membranes with a PEG-free solution so that the viruses detach from the cellulose.
Although the production and purification of viruses is the speciality of Reichl's group, the Magdeburg researchers are also involved in the search for suitable immunogens. In particular, they are investigating the glycosylation of the spike S1 protein on the surface of the coronavirus. This protein is not displayed nakedly on the surface of the virus, but is instead covered with sugar molecules (i.e., it is glycosylated).
Which immune response is caused by differently glycosylated spike proteins?
"Glycosylation could strongly influence the effectiveness of a vaccine against the coronavirus," says Reichl. "With some viruses, such as the flu virus, this varies greatly. However, relatively little is known about the corona virus."
Together with Achim Kaasch and Dunja Bruder, professors from the Medical Faculty of the University of Magdeburg, and the company glyXera GmbH, which he co-founded as a spin-off of the Max-Planck-Gesellschaft, he seeks to change this. The scientists will first produce the spike S1 protein in insect cell cultures, specifically modify glycosylation using synthetic biotechnology methods, and investigate the immune response in mice. If it turns out that a spike S1 protein with a specific sugar envelope prepares the immune system particularly well for an infection with SARS-CoV-2, it could help the scientists to develop an effective vaccine.
It still remains open as to which vaccine will ultimately be used against SARS-CoV-2 and which process will be used to produce it. "With our work, we want to help create more options so that we end up with a vaccine that is as effective as possible and which can be produced in large numbers," says Reichl. "We hope that the COVID-19 pandemic can soon be contained with vaccination and that efficient methods for supplying the world population with inexpensive vaccines will be available for similar challenges."




















