Mimicking a chronic immune response changes the brain
As March comes around, many people experience hay fever. As excessive immune responses go, most would admit that hay fever really isn't that bad. At the other end of the spectrum are severely debilitating autoimmune diseases like rheumatoid arthritis and multiple sclerosis. A common thread in all these conditions are cytokines, molecules that cause inflammation. Recent research by the University of Tsukuba sheds light on the effect of excessive cytokines on neuronal and glial cells in the brain.
Researchers led by Professor Yosuke Takei and Assistant Professor Tetsuya Sasaki at the University of Tsukuba in Japan have been studying an important cytokine called interleukin (IL)-17A. Their recent study shows that chronic increases in the levels of IL-17A circulating in mouse blood can reduce the microglia activity in one part of the brain's hippocampus. This might explain why it's related to several neurological diseases.
The researchers focused on IL-17A because it is known to be involved in neurological autoimmune disorders as well as disorders of the mind. "In addition to being linked to multiple sclerosis," explains Sasaki, "recent reports show that IL-17A is also a factor in Alzheimer's disease, schizophrenia, and autism spectrum disorder." To study how chronically high levels of IL-17A can affect the brain, the team used their knowledge of how IL-17A is made naturally in the body.
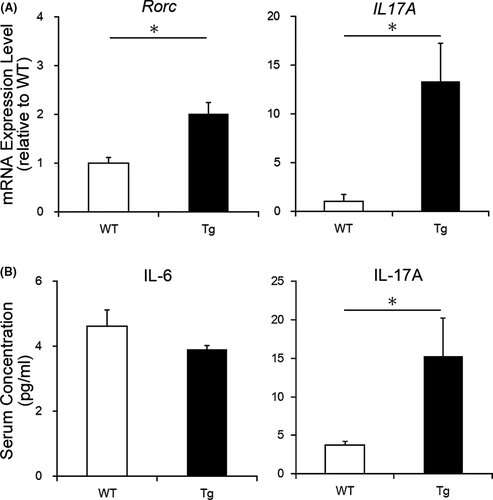
The researchers focused on immune cells called helper T-cells. Helper T-cells come in many varieties, each one making its own cytokine, and each one created from a generic helper T-cell. "Our strategy," says Sasaki, "was to induce more generic helper T-cells to become the kind that produce IL-17A." With more of these helper T-cells, called Th17, the mutant mice did indeed produce more IL-17A in the gut, which spread throughout the body in the blood.
IL-17A is known to interact with two kinds of glial cells in the nervous system, astrocytes and microglia. The researchers found that chronically high IL-17A led to reduced activity and density of microglia in one region of the hippocampus, a part of the brain that is needed for learning and forming memories. In contrast, astrocytes in the brain did not differ between the mutant and control mice. Thus, there was reason to believe that chronic IL-17A inflammation would affect cognition, specifically memory. Surprisingly, spatial memory seemed to be just as good in the mutant mice as in the control mice.
"These mutant mice can be used in future studies as a model for chronic IL-17A-related inflammation," says Takei. "Further neuronal and behavioral testing will help us begin to understand IL-17A's role in a range of debilitating neurological disorders."
More information: Tetsuya Sasaki et al. Effects of RORγt overexpression on the murine central nervous system, Neuropsychopharmacology Reports (2021). DOI: 10.1002/npr2.12162

















