Immune memory less durable after severe COVID-19, study suggests
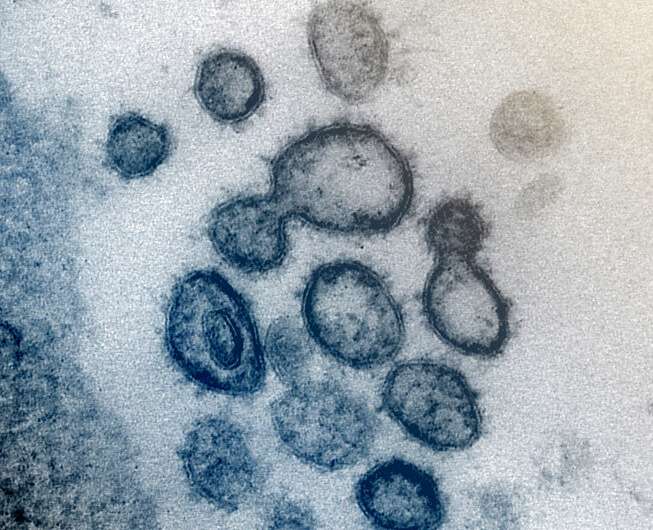
Infection-fighting B cells retain better memory of the coronavirus spike protein in University Hospital patients who recover from less-severe cases of COVID-19 than in those recovering from severe COVID-19, a new study suggests. Findings by scientists from The University of Texas Health Science Center at San Antonio were published Wednesday (Dec. 22) in the journal PLOS ONE.
Evelien Bunnik, Ph.D., corresponding author of the paper, said the results hint of subtle differences in the quality of immune response based on COVID-19 severity. Dr. Bunnik is an assistant professor of microbiology, immunology and molecular genetics at the health science center, also referred to as UT Health San Antonio.
The study focused on memory B cells that react against the SARS-CoV-2 spike protein. Blood samples were analyzed one month after symptom onset and five months post-onset. After one month, a significant proportion of spike-specific B cells were active.
However, samples from eight individuals who recovered from less-severe disease showed increased expression of markers associated with durable B cell memory as compared to individuals who recovered from severe disease, the authors wrote. The markers include T-bet and FcRL5.
T-bet-positive, spike-specific B cells nearly disappeared from the blood samples five months post-symptom onset, the authors noted. Overall, a more dysfunctional B cell response is seen in severe disease cases, they wrote.
Non-severe cases were defined as not requiring supplemental oxygen or invasive ventilation, while severe cases needed invasive mechanical ventilation or extracorporeal membrane oxygenation (ECMO). "The definition of severe disease was made based on the need for mechanical ventilation or ECMO, because this distinguishes the most critical patients, who are the most likely to develop impaired immune responses," said study senior author Thomas Patterson, MD, professor and chief of infectious diseases at UT Health San Antonio who leads COVID-19 care at clinical partner University Health.
Study participants were enrolled in the Adaptive COVID-19 Treatment Trial (ACTT)-1 or ACTT-2 clinical trials. Samples were from University Health patients co-enrolled in the UT Health San Antonio COVID-19 Repository.
"The increased percentage of B cells associated with long-lived immunity in non-severe COVID-19 patients may have consequences for long-term immunity against SARS-CoV-2 re-infection or severity of the resulting disease," the authors wrote.
More information: Raphael A. Reyes et al, SARS-CoV-2 spike-specific memory B cells express higher levels of T-bet and FcRL5 after non-severe COVID-19 as compared to severe disease, PLOS ONE (2021). DOI: 10.1371/journal.pone.0261656

















