Early add-on therapy with PCSK9 inhibitor appears safe in patients post heart attack
Compared with a placebo, the addition of the injectable cholesterol-lowering drug alirocumab to high-intensity statin treatment in patients who have had a heart attack resulted in twofold greater reductions in three key measures of plaque vulnerability that signal risk for future cardiac events, according to research presented at the American College of Cardiology's 71st Annual Scientific Session.
The trial is the first to examine the effect of the PCSK9 inhibitor alirocumab on "vulnerable plaques" (fatty deposits in arteries that are considered likely to cause future cardiac events) using three imaging tests that assess the probability of future cardiac events in patients recovering from a heart attack. The study met its primary endpoint—a reduction in percent atheroma volume (PAV), which is a measure of cholesterol plaque buildup in the coronary arteries.
"Following early initiation of alirocumab on top of high-intensity statin therapy in a high-risk population with acute myocardial infarction, we observed a twofold regression of coronary atherosclerosis and stabilization of high-risk plaques when compared with treatment with statins alone," said Lorenz Räber, MD, Ph.D., professor of cardiology and director of the catheterization laboratory at Bern University Hospital in Switzerland and the trial's principal investigator.
Most heart attacks are caused by cholesterol deposits in the coronary artery that are covered by a thin, fibrous cap. A rupture in this cap can potentially lead to a coronary blockage that results in a heart attack.
About 1 in 5 people who have had a heart attack will be readmitted to the hospital with a second cardiac event within five years.
PCSK9 inhibitors boost the ability of the liver to clear low-density lipoprotein (LDL) cholesterol—or "bad" cholesterol—from the body, thereby lowering levels of LDL cholesterol in the blood. Alirocumab, which is injected under the skin, was the first drug in this class to be approved by the U.S. Food and Drug Administration for use either alone or in combination with other cholesterol-lowering medications such as statins.
The current trial, known as PACMAN-AMI, enrolled 300 patients who had a heart attack and were treated with a stent (a tiny mesh tube) to open the blocked artery. The patients' average age was 58.5 years and 81.3% were men. All patients received a high daily dose of the statin drug rosuvastatin (20 mg), and they were randomly assigned to receive injections of either alirocumab or a placebo every two weeks as additional treatment. The first injection was administered less than 24 hours after the insertion of a stent, while patients were still in the hospital for their heart attack.
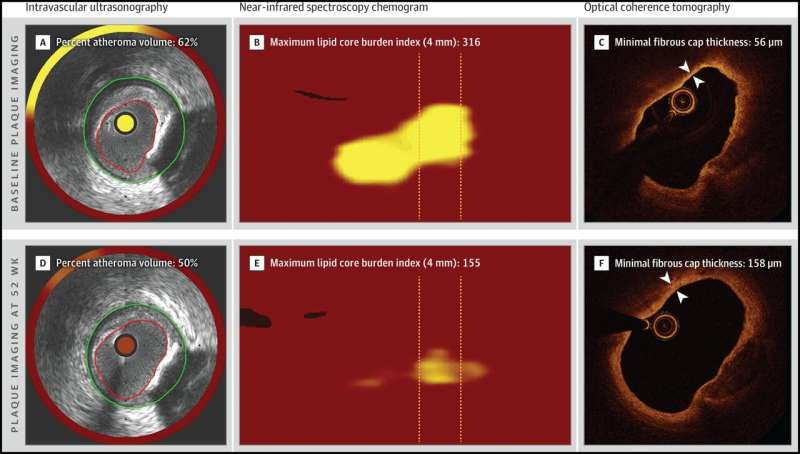
Within 24 hours of the stenting procedure, patients underwent three types of imaging in two other arteries to the heart (not including the one that had caused the heart attack). These imaging tests measured the amount of plaque buildup (PAV, the primary endpoint) by intravascular ultrasound; the amount of cholesterol within the plaques by near-infrared spectroscopy; and the thickness of the hard outer layer, or cap, covering the plaques by optical coherence tomography (a light-based imaging technique that provides microscopic images of the artery). The thinner the hard cap is, the more likely it is to rupture, which could allow the plaques to block the artery and cause another heart attack.
"PAV, cholesterol content of the plaque and cap thickness are key characteristics of vulnerability to future cardiac events," Räber said. "This kind of detailed information could previously be obtained only at autopsy. Nowadays, it can be visualized in living patients using these imaging tests. Our study was the first to use three intracoronary imaging tests in combination to provide a comprehensive picture of plaque size, composition and morphology [shape and structure]."
Patients continued their assigned treatment for 50 weeks. At 52 weeks, the three imaging tests were repeated and the researchers analyzed the differences between before-treatment and after-treatment images. On all three imaging measures, patients who received alirocumab did significantly better than those who received a placebo. Overall plaque material and lipid deposits on their arterial walls regressed to a greater extent (twofold reduction), and the hard caps covering the plaques became thicker (twofold thickening), meaning they were less likely to rupture. Patients who had received alirocumab also needed significantly fewer repeat stenting procedures. No significant adverse events occurred in relation to the imaging tests.
Patients receiving the combination of alirocumab and a statin achieved an average LDL level of 23.6, the lowest level ever achieved in a major trial of cholesterol-lowering drugs in acute myocardial infarction patients, Räber said. The study drug was generally well tolerated (6.4% injection-site reactions and 3.4% allergic reactions).
"These findings provide insights to support more-frequent, early and targeted use of alirocumab on top of high-intensity statin therapy in patients who have had a heart attack and are at high risk for a second one," Räber said.
A limitation of the study, he said, is that it was not designed to measure whether the addition of alirocumab to statin therapy resulted in fewer cardiac events compared with statin therapy alone. Instead, the study used changes in the three imaging markers of heart attack risk as surrogate endpoints.
This study was simultaneously published online in the Journal of the American Medical Association at the time of presentation. The study was an investigator-initiated academic trial funded by grants from Sanofi and Regeneron, the co-developers of alirocumab, and Infraredx, the manufacturer of near-infrared spectroscopy imaging catheters.
More information: Lorenz Räber et al, Effect of Alirocumab Added to High-Intensity Statin Therapy on Coronary Atherosclerosis in Patients With Acute Myocardial Infarction, JAMA (2022). DOI: 10.1001/jama.2022.5218

















