Lung cancer: When radiotherapy fails
Lung cancer is the most common cancer in the world, with 2.2 million new cases and around 1.8 million deaths in 2020 alone. Although knowledge about the disease has improved considerably, and new therapeutic strategies can prolong the lives of previously incurable patients, the numbers clearly show that lung cancer is still a serious disease and the mortality rate is still far too high.
To further reduce the number of deaths from this type of tumor, novel and improved treatments are needed. Würzburg researchers are concentrating on radiotherapy. In combination with chemotherapy, this is still one of the most important treatment approaches. This is especially true for late-stage non-small cell lung tumors, where treatment options are rather limited.
PTEN mutation is suitable as a biomarker
In this type of lung tumor, radiotherapy can be ineffective. This is due to the interaction of a common, specific mutation in the PTEN gene with the DNA repair enzyme ATM, as the Würzburg team found out.
However, lung tumors, in which this mutation occurs, can be therapeutically influenced. With two experimental inhibitors, the researchers succeeded in blocking the DNA repair enzyme in the tumor cells. As a result, the tumors became sensitive to radiation again and could be killed in tumor models.
Inhibitors in preclinical testing
"Such inhibitors have not yet been approved for use in humans, but partake in clinical trials," explains cancer researcher Dr. Markus Diefenbacher from the Biocentre at the University of Würzburg. His team has published the new findings in the journal Cell & Bioscience together with a group led by radiotherapist Dr. Thomas Fischer from Professor Michael Flentje's research group at the University Hospital Würzburg.
If the inhibitors pass the clinical tests, they offer a new opportunity: the PTEN mutation is suitable as a biomarker that indicates a tumor's resistance to radiation. With corresponding analyses, one could specifically identify patients who might benefit from a combination of inhibitor and radiotherapy. This could be realized quickly: patients with non-small cell lung cancer are already routinely examined for PTEN and other disease-relevant mutations.
Focus on radiation dose reduction
Currently, several clinical trials are looking at the impact of PTEN and ATM on treatment outcomes. "We are confident that our new findings will generate a lot of interest in pursuing this innovative strategy for the treatment of non-small cell lung tumors," says Professor Michael Flentje.
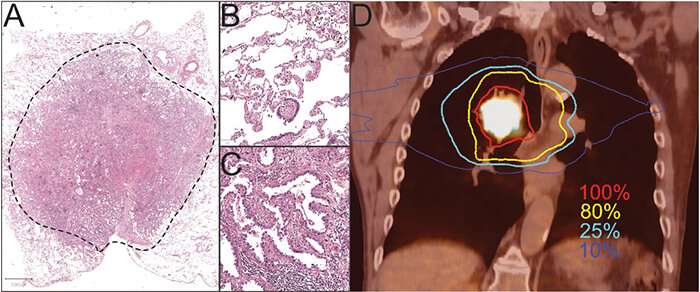
Radiotherapy is a mainstay in the treatment of late-stage tumors of the respiratory tract and other organs. The Würzburg team is therefore continuing to research new strategies and targets. One focus is on reducing the radiation dose in such a way that the desired therapeutic success is still achieved and at the same time the healthy tissue around the tumor is spared as much as possible.
More information: Thomas Fischer et al, PTEN mutant non-small cell lung cancer require ATM to suppress pro-apoptotic signalling and evade radiotherapy, Cell & Bioscience (2022). DOI: 10.1186/s13578-022-00778-7



















