The allocation of COVID-19 vaccinations in 29 countries at the beginning of 2021
A research team from the Interdisciplinary Centre for Ethics of Jagiellonian University in Kraków (Poland) has analyzed vaccination schedules published by 29 countries at the turn of 2020 and 2021, including members of the EU, UK, and Israel, with respect to the order in which they provided vaccination for different groups of citizens. The results of their research were published in the Journal of Law and Biosciences.
COVID-19 vaccinations were scarce commodities at the beginning of 2021. The common element of all vaccination policies was to prioritize health care workers as well as the staff and residents of nursing care facilities. Only ten countries had also singled out teachers as a group to be prioritized when it came to COVID-19 vaccination, and an even lesser number decided to do the same with employees of grocery stores (Austria, Germany, Ireland, Latvia, Romania, and Slovenia).
Only six countries followed the recommendation of the World Health Organization (WHO) in providing migrants, refugees, and prisoners staying in crowded conditions with priority access to vaccination (Cyprus, Germany, Greece, Ireland, Latvia, and Romania).
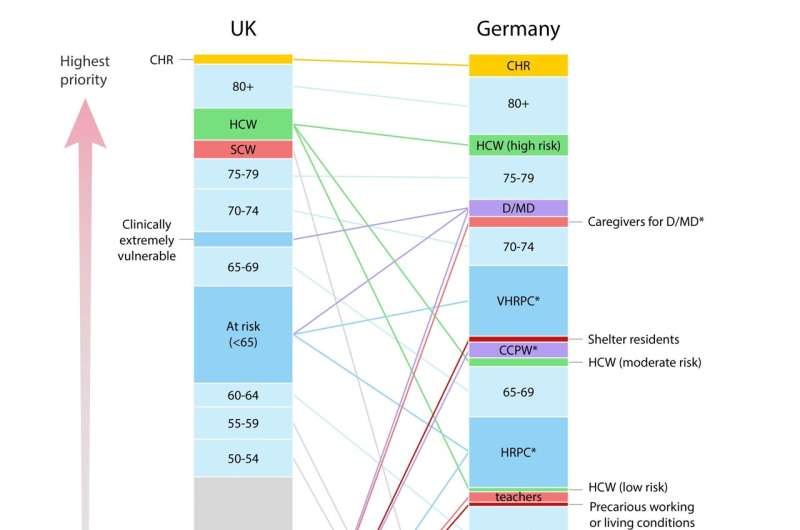
Researchers working on the project mapped out the differences in vaccination schedules. The main difference was related to the criteria on which various countries based their policies. In Great Britain, for example, the schedule was based almost solely on the age of citizens, while other countries took into account various other factors contributing to an increased risk of death from COVID-19 (e.g., comorbidities). A few countries also included an increased risk of infection as a factor (e.g., Germany).
Karolina Wiśniowska from the Interdisciplinary Centre for Ethics (INCET) observed that there is no consensus among the experts as to how preventive measures should be distributed and that official schedules on the distribution of medical prevention in the case of COVID-19 have not yet been analyzed or compared systematically.
The researchers point out that governments adopted very different strategies when it came to designing policies for vaccination schedules and when it came to designing policies for treating patients already infected with COVID-19.
In March and April 2020, several foreign medical associations published recommendations on how to distribute medical equipment and drugs in situations where resources are scarce. In particular, they mentioned access to ventilators and beds in intensive care units.
"Some of those recommendations were very controversial, as in the case of access to ventilators. Some posited we consider certain patients' probability of survival, while others suggested assessing their predicted lifespan in the future. This could lead to the exclusion of the elderly or patients with comorbidities," said Prof. Tomasz Żuradzki, head of INCET at Jagiellonian University.
The situation was different when it came to vaccination schedules. All of them prioritized groups with increased risk of death, such as the elderly, and in many cases, patients with comorbidities.
The high chance of infection was taken into account much more rarely, with the exception of law enforcement and emergency services employees as well as social workers.
Vaccination schedules for different social groups are in stark contrast with the regulations concerning the allocation of scarce healthcare resources in the cases of treatment (e.g., transplants). In this second case, the aim is not to save as many people from sudden death, but it is required to assess the procedure's feasibility based on various factors, such as the expected lifespan and quality of the future life of the patient. In most countries, these regulations about the distribution of life-saving curative resources are very similar.
"The moral judgments underlying vaccination schedules cannot be unequivocally interpreted within the light of dominant ethical frameworks. However, this ambiguity may be seen as their strong point," said Dr. hab. Wojciech Ciszewski from the Chair in Legal Theory at Jagiellonian University. "Since the public opinion and experts represent various ethical standpoints, and broad support is necessary for successful vaccination strategies, the ability to defend these strategies on various moral grounds may increase their social legitimacy," he added.
More information: Value choices in European COVID-19 vaccination schedules: how vaccination prioritization differs from other forms of priority setting, Journal of Law and the Biosciences (2022). DOI: 10.1093/jlb/lsac026





















