No need to redefine osteoporosis, concludes IOF and ESCEO position paper
A new position paper by the International Osteoporosis Foundation (IOF) and European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) addresses the rationale for separate diagnostic and intervention thresholds in osteoporosis.
In "The need to distinguish intervention thresholds and diagnostic thresholds in the management of osteoporosis" paper, the authors outline why the established WHO diagnostic criteria for osteoporosis has served the field well, and recommend that this should be retained whereas a distinction needs to be made between diagnostic and intervention thresholds. They note the successful distinction between diagnostic and intervention thresholds in the cardiovascular field.
Professor John Kanis, lead author and Honorary President of IOF, states, "The enormous treatment gap in the management of patients at increased risk of fractures, including in patients who have already fractured, is a major problem. The reasons for this are many, including a lack of awareness among physicians and the patients themselves."
"It has however been suggested that the fault lies with the diagnostic definition of osteoporosis as defined by the WHO in 1994. This has resulted in some arguing that a change in the diagnostic criteria would improve the low rate of treatment in patients who are at high risk."
"While the intention is laudable, we find that a change in definition is problematic and that there is little evidence that this alone would improve management."
The WHO diagnostic definition of osteoporosis is a bone mineral density (BMD) that is 2.5 standard deviations (SD) or more below the mean value of young healthy women i.e., a T-score ≤-2.5 SD. The definition provided a standardized description that allowed the comparison of osteoporosis prevalence across countries and regions, and secular trends. The definition of osteoporosis rapidly won general acceptance, shown by its almost immediate use in clinical practice and research, and by its adoption as inclusion criteria for drug trials.
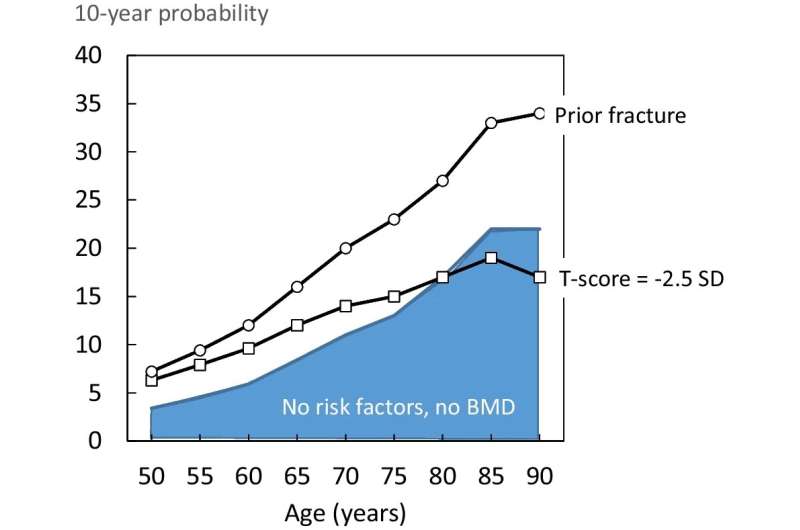
Notwithstanding these advantages, it is now clear that BMD alone is a poor screening tool and is not ideal as an intervention threshold. The majority of individuals who sustain a fragility fracture do not have a BMD in the osteoporosis range. This is comparable to the relationship between hypertension and stroke where high blood pressure is an important cause of stroke, but the majority of individuals with stroke are not hypertensive. In addition, a given T-score threshold has a different significance at different ages and countries.
With this new awareness, the osteoporosis field has moved towards fracture risk assessment, with or without BMD, to set intervention thresholds. The position paper describes the increasing use of prior fracture and FRAX probability (the most widely used fracture risk assessment tool) as an intervention threshold.
Professor Jean-Yves Reginster, co-author and President of ESCEO, stated, "The use of intervention thresholds based on fracture probability is increasingly implemented into routine clinical practice, but this does not minimize the value of the current diagnostic criteria which allows us to quantify the burden of disease. The operational BMD-based definition, unique in the musculoskeletal field, is completely in accord with clinical expectations of the burden of the disorder."
"It is analogous to that employed successfully for the use of continuously distributed clinical risk variables in the management and prevention of other multifactorial outcomes such as myocardial infarction (by defining hypercholesterolaemia) and stroke (by defining hypertension). It has yielded a regulatory framework in the U.S., EU and elsewhere which has permitted the development of a wide range of therapeutic interventions."
Professor Kanis concluded, "The operational BMD-based definition is a triumph in healthcare, and there is no intellectually sound reason to argue for a change at present. We recommend that the BMD-based definition of osteoporosis be retained whilst further clarity is brought to bear on the distinction between diagnostic and intervention thresholds, as has been successfully managed in cardiovascular disease."
The findings were published in Osteoporosis International.
More information: John A. Kanis et al, The need to distinguish intervention thresholds and diagnostic thresholds in the management of osteoporosis, Osteoporosis International (2022). DOI: 10.1007/s00198-022-06567-9



















