This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
New pain medications are still widely inaccessible to individuals living with sickle cell disease
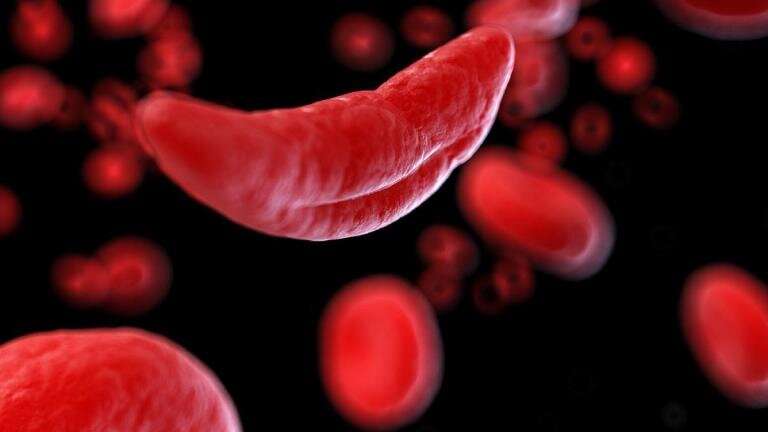
Sickle cell disease (SCD), a rare chronic, progressive, life-threatening, inherited blood disorder, often affects individuals with chronic pain that can be debilitating to their quality of life. Yet less than 4% of people living with SCD who experience chronic pain episodes have prescriptions for newer FDA-approved pain-relieving drugs, including l-glutamine, voxelotor, and crizanlizumab, according to a new study published in Blood Advances.
Further, researchers found that less than a third of patients with pain episodes have prescriptions for hydroxyurea, a drug commonly taken to reduce pain caused by sickle cell disease.
SCD affects more than 100,000 Americans and an estimated 100 million persons worldwide. According to the Centers for Disease Control and Prevention (CDC), SCD affects one out of every 365 Black or African American births and one out of every 16,300 Hispanic American births.
The condition can cause severe pain, joint and organ damage, and stroke. Advances in SCD research have prompted the development of groundbreaking therapies, allowing 93% of young people with SCD to live into adulthood, a statistic marking tremendous progress in disease interventions over the last few decades.
While individuals are now living significantly longer, those with frequent pain episodes still face challenges with quality of life, a barrier that pain-relieving medications intend to relieve.
Prior to 2017, hydroxyurea was the only pain-relieving medication available for patients with sickle cell disease developed to help the body make rounder, less sickled cells, which ultimately aims to reduce the overall number of pain episodes an individual experiences. In the last few years, several new therapies, including l-glutamine, voxelotor, and crizanlizumab, have gained FDA approval. Despite the growing list of options to prevent SCD-associated vaso-occlusive pain episodes, many patients still lack access to and knowledge of these drugs.
"These medications are FDA approved, and yet, patients are very rarely using them. Our findings suggest that roughly 2-4% of patients eligible for these medications have a prescription for one of these medications, and less than 2% are being prescribed combination therapy," explained Robert Cronin, MD, of The Ohio State University Department of Internal Medicine. "We knew disparities in the use of these drugs existed, but it's been eye-opening to see just how wide these gaps are."
To conduct this study, investigators surveyed data collected between 2016-2020 from the IBM Watson MarketScan Administrative billing database. They analyzed inpatient and outpatient data, emergency department encounters, total encounters with an SCD diagnosis, procedure codes, and prescription data. Individuals who had visited a health care provider at least three times and had a confirmed SCD diagnosis were included in the study.
Using this data, researchers then assessed patient use of hydroxyurea, l-glutamine, voxelotor, and crizanlizumab, both alone and concurrently, sorting by age group and geographic region.
Researchers found that hydroxyurea was the most prominently prescribed medication (31.5%), followed by l-glutamine (3.2%), then crizanlizumab (2.3%) for vaso-occlusive pain. Voxelotor is only approved for people with lower hemoglobin levels and was prescribed to 2.9% of the population. Authors also found that patients living in rural areas had significantly lower use of medications approved for pain episodes, compared to those in non-rural communities.
Finally, less than 3% of the population used any type of combination therapy to treat pain, while 0.3% used combinations of these newer FDA approved treatment options.
Importantly, all patients included in this study had private insurance plans. Most individuals with SCD are covered by public insurance plans, suggesting that these findings may be even more disparate among a more representative population. Further, investigators solely tracked prescription patterns and did not track medication adherence. Understanding how often these medications are utilized after being prescribed could be useful in garnering the full picture of SCD medication inequities.
"I think it is important that we educate both providers and patients about the options that exist to treat their condition," said Dr. Cronin.
"From a provider standpoint, it's essential that a spectrum of physicians possess knowledge of sickle cell disease and its available treatment options. A lot of patients, especially those living in rural areas, do not always have access to a hematologist. And then from the patient standpoint, providing patient-friendly material that allows them to be knowledgeable about their disease and advocate for themselves can help improve care for this population."
More information: Robert M Cronin et al, The Use of FDA-Approved Medications for Preventing Vaso-Occlusive Events in Sickle Cell Disease, Blood Advances (2023). DOI: 10.1182/bloodadvances.2022008965



















