This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Study: Survivors of stroke do better on general practitioners' chronic disease management plans
A study has confirmed that government policies funding general practitioners (GPs) to provide structured chronic disease management improve long-term survival following stroke and stroke-like symptoms.
Published in The Lancet Regional Health—Western Pacific, the Monash University-led study was developed to determine the effectiveness of government-funded chronic disease management policies to improve long-term outcomes—survival, hospital presentations, and preventive medication adherence—following stroke/Transient Ischemic Attack (temporary stroke-like symptoms).
Stroke is a lifelong condition, making it the third greatest cause of global Disability Adjusted Life Years and second for those aged 50 and over. Survivors of stroke have an elevated risk of recurrent stroke (approximately 11% at one year, 26 at five years), and most have additional comorbid conditions such as high blood pressure and diabetes.
The 12,386 participants were identified through the Australian Stroke Clinical Registry (January 2012–December 2016) from 42 hospitals in Victoria and Queensland. Registry data was linked with state and national hospital, general practice, pharmaceutical, aged care, and death datasets. Registrants living in the community, not receiving palliative care, and who survived to 18 months following stroke/TIA were included.
Forty-five percent of participants had a chronic disease management plan. Those with a plan had 26% improved survival over the 12 months follow up and 16%–23% improved preventative medication adherence. Despite the health benefits, less than half of the cohort had received a chronic disease management plan.
The study is the only national evaluation of a primary care policy aimed at incentivizing GPs to provide structured and comprehensive chronic disease management.
Clive Kempson, from Clyde North in Victoria, participated in the study and had a chronic disease management plan. Clive, 59, survived a stroke just over seven years ago and felt abandoned by the system after a short stint in rehab.
Once given a management plan he felt supported and was able to receive essential medical care relevant to stroke survival and other conditions he lives with.
"With my management plan I felt empowered and involved in my health recovery. I asked lots of questions of my GP so I knew what was going on," Clive said.
"Health Department decision makers don't consider the long-term view. Having a management plan is essential to recovery and I feel very grateful to have one. I also advocate for other stroke survivors as a way of giving back."
Project lead and author, Associate Professor Nadine E. Andrew, is from Monash University's Central Clinical School and a Research Data Lead for the National Center for Healthy Aging.
"Our findings provide evidence of the population effectiveness of Australian Medicare-funded chronic disease management policies in primary care for improving the long-term survival of people living with stroke/TIA and adherence to secondary prevention medication," she said.
"We provide evidence of survival benefits afforded by government policies that financially support primary care physicians to provide structured chronic disease management in the long-term management of stroke/TIA.
"We also provide a strong case for the ongoing provision of these plans within a universal health care system. Strategies to improve uptake at the GP level are needed and could include greater financial incentives and mandates, education for patients and health care professionals, and ongoing population monitoring involving audit and feedback."
Co-investigator Associate Professor Monique Kilkenny, from the School of Clinical Sciences at Monash Health, strongly advocates for "efforts to ensure quality of care provided to patients with stroke for improvement of health care and patient outcomes."
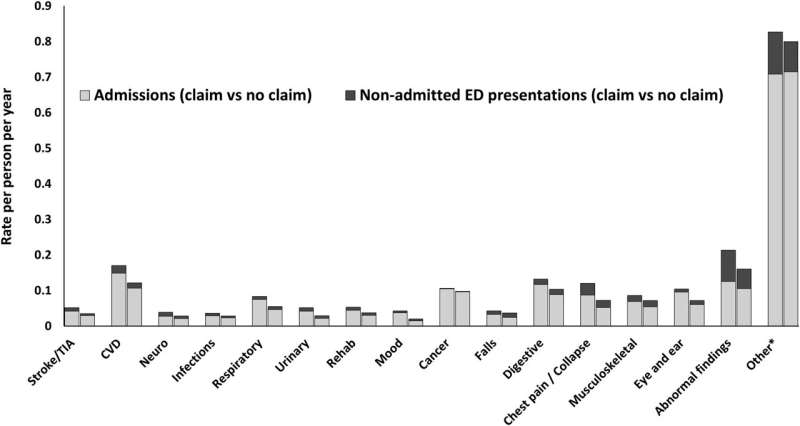
"The increase in overall hospital presentations represent an informed patient cohort more able to recognize the need for presentation to hospital," she said.
More information: Nadine E. Andrew et al, The population effect of a national policy to incentivize chronic disease management in primary care in stroke: a population-based cohort study using an emulated target trial approach, The Lancet Regional Health—Western Pacific (2023). DOI: 10.1016/j.lanwpc.2023.100723




















