This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Researchers develop digital test to directly measure HIV viral load
A milliliter of blood contains about 15 individual drops. For a person with human immunodeficiency virus (HIV), each drop of blood could contain anywhere from fewer than 20 copies of the virus to more than 500,000 copies. Called the viral load, this is what is measured to allow clinicians to understand how patients are responding to anti-viral medications and monitor potential progression.
The time-consuming viral load testing needs to be repeated several times as a patient undergoes treatment. Now, a Penn State research team has developed a time and cost-efficient digital assay that can directly measure the presence of HIV in single drop of blood. They published the work in ACS Nano.
According to the corresponding author Weihua Guan, associate professor of electrical engineering and biomedical engineering in the Penn State College of Engineering, the digital assay is the first step in providing a clinical diagnostic tool for a bevy of infectious diseases.
Conventional tests for HIV viral load involve taking genetic material from the sample, amplifying it and comparing it to reference samples. The gold standard test, called RT-PCR, can produce a close estimate of the actual viral load, but it is not a direct measurement. Guan and his team took a more direct approach with their test, named Self-digitization Through Automated Membrane-based Partitioning (STAMP), which is less expensive, quicker and requires less blood than the RT-PCR.
"Here's how it works: We take a small sample of a person's blood and extract the viral RNA—the genetic material of the virus—from it," Guan said. "We then mix this RNA with a special protein called Cas13, which is part of the CRISPR system."
CRISPR-Cas13 is a "revolutionary tool," Guan said, that enables researchers to target and manipulate RNA sequences. In this study, the researchers are leveraging the technology not for its editing capabilities, but for its diagnostic potential. They are using CRISPR-Cas13 to detect and signal the presence of HIV.
Once the RNA is combined with Cas13, the researchers place a nanopore polycarbonate membrane—a thin filter that is readily available, making it a cost-effective material, Guan said—on the mixture. The nanopores are so tiny that they can partition the mixture into single droplets containing only one RNA molecule, which has the Cas13 protein attached. If HIV is in the RNA molecule, the Cas13 protein—which is activated by HIV RNA—will cut reporting molecules, generating a signal the researchers can detect.
"By counting the number of droplets showing this signal, we can determine the amount of HIV in the person's blood," Guan said. "The more droplets with the signal, the higher the viral load."
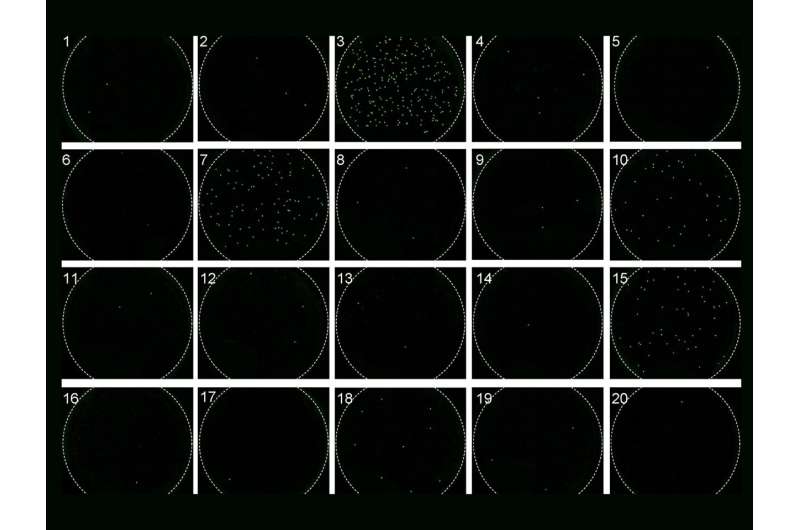
The researchers tested this approach with synthetic HIV RNA to optimize the assay for sensitivity and accuracy before testing laboratory plasma and eventually patient plasma samples. They validated the STAMP method by quantifying HIV viral loads in 20 patient plasma samples with comparable accuracy to the traditional RT-PCR method, which typically requires more blood. Guan said they are working on procuring more samples to continue their testing.
The team also found that the approach can provide an accurate assessment for HIV viral loads at or higher than about 2,000 virus copies per milliliter of blood. A viral load is considered low when there are fewer than 10,000 copies of the virus per milliliter; undetectable at 20 copies or fewer; and high at roughly 100,000 copies but can extend beyond a million.
According to Guan, the 2,000 to 10,000 detection range can be important for clinicians monitoring patients for viral rebound. People undergoing antiretroviral therapy (ART) can achieve undetectable virus levels, meaning they can no longer sexually transmit the virus, but rising virus levels can indicate an individual is developing ART resistance or another issue.
"While further improvements are needed to enhance its detection limit and automate the setup, the STAMP-based digital CRISPR method shows great potential for advancing HIV viral load monitoring," Guan said, explaining that the researchers plan to continue improving the platform's efficiency and accuracy to quantify multiple viruses, with the eventual goal of bringing the device to market.
More information: Reza Nouri et al, STAMP-Based Digital CRISPR-Cas13a for Amplification-Free Quantification of HIV-1 Plasma Viral Loads, ACS Nano (2023). DOI: 10.1021/acsnano.3c01917



















