This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Scientists discover pathogenic mechanism and novel treatment for Klebsiella pneumoniae
Two novel approaches for the treatment of infections caused by antibiotic-resistant superbugs have shown efficacy and good clinical application potential in studies performed by a team from The Hong Kong Polytechnic University (PolyU). Their findings have recently been published in Signal Transduction and Targeted Therapy and the Journal of Infection.
The World Health Organization has repeatedly warned that the emergence and spread of multidrug-resistant microbes, commonly known as superbugs, could lead to the next wave of public health disasters. Many of the known superbugs actually evolved from normal flora, or bacteria that commonly exist in our body, and may cause a wide range of infections, especially when our immune system is weakened; hence they may readily spread in the hospital and the community, and potentially pose a threat which is more serious and long-lasting than the COVID-19 pandemic.
To date, a number of bacterial strains have been classified as superbugs, among which the hyper-resistant and hypervirulent Klebsiella pneumoniae is arguably the one which poses the greatest threat to human health. In 2017, a research team led by Prof. Chen Sheng, Chair Professor of Microbiology, Member of State Key Laboratory of Chemical Biology and Drug Discovery, and Head of Department of Food Science and Nutrition at PolyU, discovered a newly emerged genetic variant of Klebsiella pneumoniae, namely the hyper-resistant and hypervirulent Klebsiella pneumoniae (CR-hvKP), which can cause untreatable and fatal infections even in healthy individuals.
As the name implies, this superbug is not only multidrug-resistant, but also highly invasive. Various studies in China showed that the mortality rate of CR-hvKP infection ranged from 25% to 45%. To date, CR-hvKP has been regarded as an "urgent threat to human health" by many medical experts worldwide.
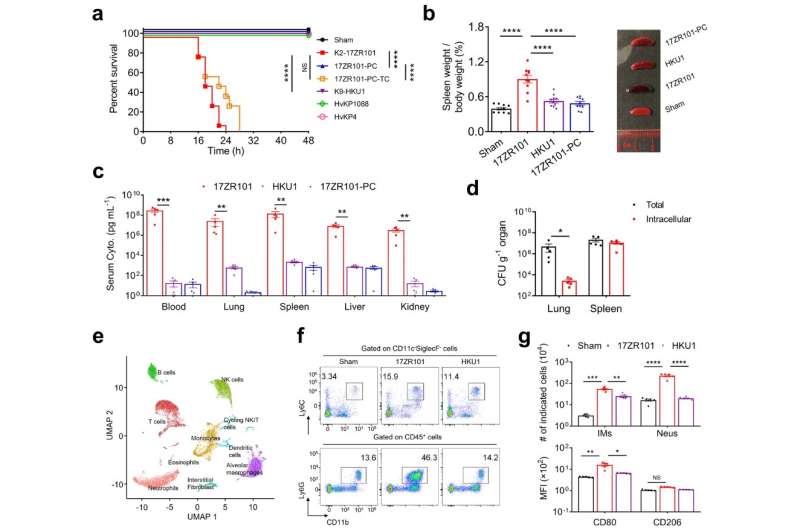
After several years of intensive research, the research team has recently made major breakthroughs in their efforts to delineate the pathogenic mechanism of CR-hvKP and devise effective intervention strategies. The team also identified the key factors involved in interaction with the host and the nature of the host immune response triggered during the process of infection. Specifically, they discovered the signal pathways through which the pathogen triggers the onset of a cytokine storm, in which the signal molecules can induce uncontrolled activation of immune cells of the host that can eventually develop into septic shock, an extremely dangerous and potentially fatal condition.
Subsequent experiments revealed that inhibiting the onset of a cytokine storm could significantly reduce mortality among infected patients. The research team studied the therapeutic value of immunosuppressants such as Acetylsalicylic acid (ASA), and found that ASA can suppress the onset of a cytokine storm in infected mice. ASA, commonly known as Aspirin, is widely used to relieve mild to moderate pain and inflammation. ASA treatment can effectively suppress the infiltration of inflammatory cells into the lungs and drastically reduce cytokine production, decreasing the likelihood of septic shock in the host.
This is the first time it has been discovered that immunosuppressants can be used in the treatment of CR-hvKP infection. The new findings provide important insights into the development of new approaches for clinical management of diseases caused by this important pathogen.
However, although ASA can protect patients against septic shock during CR-hvKP infection, this compound is unable to eradicate the pathogen. The research team therefore explored the use of a combination of ASA and other antibiotics in the treatment process and found that the therapeutic effect of ASA can be further enhanced by including an effective antimicrobial agent during treatment. However, since CR-hvKP exhibits resistance to almost all known antimicrobial agents and searching for new antimicrobial compounds is not a practical way to address the problem, Prof. Chen's team adopted a "drug repurposing" approach in a separate but related study, in which they searched for over-the-counter drugs that exhibit antimicrobial effect or can act synergistically with currently used antibiotics and enhance their activity.
The team successfully identified a drug called zidovudine, which is an anti-Human Immunodeficiency Virus (HIV) agent, which can act synergistically with the antibiotic rifampicin to eradicate CR-hvKP. The advantage of identifying new antimicrobial compounds through drug-repurposing is that the drugs do not have to go through a lengthy drug development and approval process. It is expected that the zidovudine / rifampicin combination can be used alongside immunosuppressants to treat life-threatening CR-hvKP infections.
In summarizing the new research findings, Prof. Chen said, "We are glad that our studies were able to identify two promising therapeutic options that may be used alone or in combination to combat the growing threat of Klebsiella pneumoniae, only five years after we discovered the CR-hvKP strain. It should be noted that prompt treatment will reduce mortality and the spread of the pathogen."
He also added, "We plan to validate our findings in clinical trials in the near future and we believe our research efforts will eventually benefit patients and significantly reduce the mortality rate of CR-hvKP infected patients."
More information: Qi Xu et al, Molecular mechanisms underlying the high mortality of hypervirulent Klebsiella pneumoniae and its effective therapy development, Signal Transduction and Targeted Therapy (2023). DOI: 10.1038/s41392-023-01490-9
Hongyuhang Ni et al, A novel clinical therapy to combat infections caused by Hypervirulent Carbapenem-Resistant Klebsiella pneumoniae, Journal of Infection (2022). DOI: 10.1016/j.jinf.2022.05.004



















