This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
SARS-CoV-2 infects liver, stimulating glucose production and contributing to severe form of COVID-19, study shows
Research conducted at the University of São Paulo (USP) in Brazil shows that SARS-CoV-2, the virus that causes COVID-19, can infect liver cells (hepatocytes), stimulating glucose production and leading to a condition similar to diabetes (hyperglycemia) in hospitalized patients, even if their blood sugar level was normal before they were admitted to hospital.
An article on the study is published in Proceedings of the National Academy of Sciences. The findings describe part of the mechanism used by the virus to infect liver cells and impair glucose metabolism, and point to possible strategies to avert a deterioration in the clinical condition of these patients.
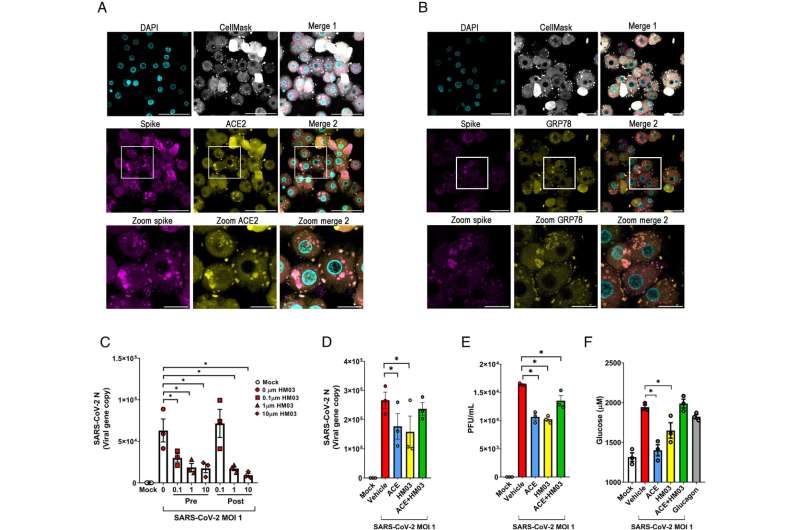
According to the researchers, viral entry into liver cells is partially mediated by cooperation between the proteins GRP78 and ACE2. The latter, known to permit cell invasion by the virus throughout the body, is present on the surface of human liver cells in a low molecular weight isoform instead of the regular one. This is one of the researchers' novel findings. Previous studies suggested liver cells did not express ACE2.
"Hyperglycemia is a prevalent complication in hospitalized COVID-19 patients that occurs regardless of their diabetes history and is associated with a worse clinical outcome," the authors write, adding that whether SARS-CoV-2 directly triggers hyperglycemia was previously unknown. They, therefore, set out to discover whether and how the virus infects hepatocytes and increases glucose production, causing hyperglycemia.
Since the start of the pandemic in 2020, diabetes has been considered a risk factor for COVID-19 patients, but the precise reasons have remained unclear. Prior research showed that the risk of death for COVID-19 patients with type 1 diabetes was 3.5 times greater than for patients without the disease. For patients with type 2 diabetes, the risk was twice as great.
"Confirming the link with receptors GRP78 and ACE2 was the cherry on the cake for our study, but the most significant result was that SARS-CoV-2 causes hyperglycemia directly, regardless of corticoid use, stress due to hospitalization, body weight and diabetes. It's the first time the virus has been shown to cause hyperglycemia directly," Luiz Osório Silveira Leiria, last author of the article, told Agência FAPESP. Leiria is a professor in the Department of Pharmacology at the University of São Paulo's Ribeirão Preto Medical School (FMRP-USP).
Hyperglycemia in type 1 diabetes may occur when the immune system attacks the cells of the pancreas that produce insulin, reducing or eliminating its capacity to secrete the hormone and leading to glucose metabolism imbalance. However, the researchers found that the patients analyzed had no pancreatic damage and therefore investigated their livers. Among other functions, the liver plays a major role in maintaining normal blood sugar levels by regulating glucose production (gluconeogenesis) and storing ingested glucose as glycogen for use when needed.
Long road
A retrospective clinical trial, combined with ex vivo and in vitro assays involving liver cells isolated from patients, showed that SARS-CoV-2 infects hepatocytes by binding to ACE2 and GRP78 receptors and increases production of hepatic glucose.
The study sample comprised 269 patients treated in the intensive care unit of Hospital das Clínicas (HC), the general and teaching hospital complex run by FMRP-USP, and 663 patients admitted with suspected COVID-19 to the Center for Intensive Medicine (CEPETI) in Curitiba, Paraná state, between March and August 2020 and submitted to PCR testing.
The control group consisted of patients with other respiratory diseases, admitted to intensive care in the same period. "We succeeded in obtaining an almost perfect control group, with similar symptoms, negative PCR results and the same hospital environment," Leiria said.
The analysis of human primary hepatocytes showed that the cells were infected by SARS-CoV-2. "We also analyzed biopsies and found the virus in these hepatocytes. It was replicating in both cases. This was most interesting, mainly because the virus didn't cause the death of these hepatocytes but used them to replicate and also increased the amount of glucose produced," he said.
After these results were obtained, their behavior was analyzed in vitro in response to other variants of SARS-CoV-2, such as delta, gamma and omicron, and the outcomes were similar.
To explore possible treatment strategies, the researchers tested compounds capable of inhibiting GRP78 and ACE2. One of the candidates confirmed was metformin, a drug used to treat high blood sugar levels in type 2 diabetes by inhibiting hepatic gluconeogenesis.
"Other studies found that intensive therapy with insulin in the hospital doesn't necessarily help these patients. A drug like metformin is more effective than insulin. Of course, metformin acts in various ways, but it's a potential route to provide additional protection for these patients," Leiria said.
On May 5, 2023, the World Health Organization (WHO) announced that it no longer considered the COVID-19 pandemic a global health emergency after a little more than three years. The pandemic caused trillions of dollars in economic losses and some 7 million deaths worldwide, according to official data. In Brazil, the number of deaths in Brazil reached at least 704,000 and there were some 37.7 million cases of COVID-19, according to the Ministry of Health's Coronavirus Panel.
Origins
The study began in 2020 when diabetes and obesity were considered the main risk factors for the more severe forms of COVID-19. "The trigger was the insight that this diabetic condition might be aggravated in the hospital," Leiria recalled. "At the time, a Brazilian article came out showing that the virus replicated more intensely in infected monocytes as more glucose was added to the culture medium."
He was referring to the discovery that higher levels of blood sugar in diabetic patients are captured by monocytes, a type of defense cell, and serve as a source of additional energy for the virus to replicate more than in a healthy organism. In response to the increased viral load, the monocytes release large amounts of pro-inflammatory cytokines with several effects, including lung cell death.
Last year Leiria's research group joined a task force led by scientists affiliated with the State University of Campinas (UNICAMP) and FMRP-USP who studied the link between visceral fat (fat around the liver, intestines and other vital organs) and severe COVID-19, concluding that it can contribute more to the severe form of the disease than subcutaneous fat.
In July 2020, another research group, led by the principal investigator for this study, Marcelo Mori, a professor at UNICAMP's Institute of Biology (IB), was the first to show that SARS-CoV-2 can infect human fat cells and that adipose tissue may be a reservoir for the virus.
More information: Ester A. Barreto et al, COVID-19-related hyperglycemia is associated with infection of hepatocytes and stimulation of gluconeogenesis, Proceedings of the National Academy of Sciences (2023). DOI: 10.1073/pnas.2217119120




















