This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
New blood-pressure related measure predicts health outcomes in patients in intensive care
Critically ill patients with circulatory shock—when the heart cannot pump enough blood and oxygen to the rest of the body, often as a result of heart failure, sepsis, or hemorrhage—require close monitoring and treatment, especially to maintain adequate blood pressure to prevent injury to important organs.
A team led by investigators at Massachusetts General Hospital (MGH) in collaboration with researchers at Massachusetts Institute of Technology (MIT) recently developed a method for monitoring such patients, which may help clinicians control their blood pressure and heart function to reduce the risk of death and other negative health outcomes. The method was tested and validated in a study published in Nature Medicine.
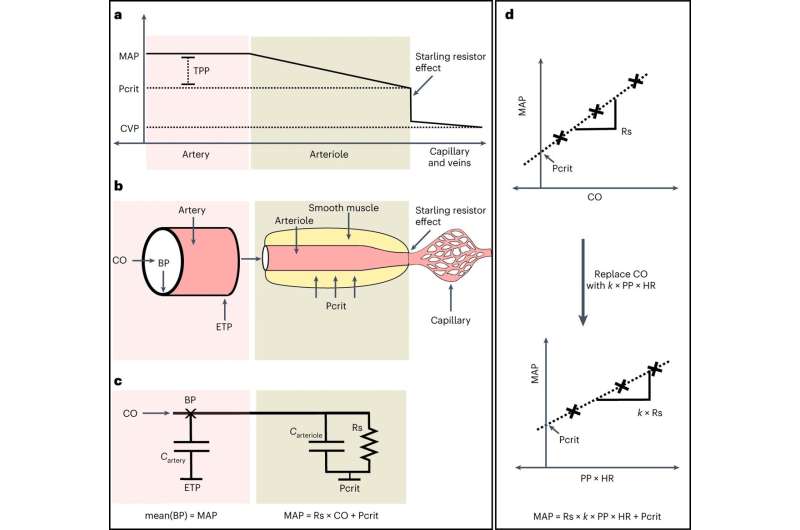
The work involved designing an approach to measure a property of the circulation called the critical closing pressure, which is the blood pressure at which small blood vessels collapse and blood flow stops. Critical closing pressure can provide an indication of blood vessel tone in response to disease and therapy, but it has not been possible to measure this parameter routinely in clinical care.
Development of the new approach utilized high resolution waveform data from blood pressure monitoring of 5,532 patients in the cardiac intensive care unit at MGH. Researchers developed an analysis based on measured parameters (including arterial pressure, pulse pressure, and heart rate) to define the critical closing pressure.
They then defined a value called tissue perfusion pressure—calculated as the difference between average arterial blood pressure and critical closing pressure—and found that it predicted a patient's risk of death, length of hospital stay, and peak blood lactate level (an indicator of tissue oxygenation).
"When treating patients with circulatory shock, it is essential to maintain adequate blood pressure targets, yet standard goals are not personalized to individual patients. We have developed a new metric that can identify individuals with inadequate tissue perfusion who are at risk for adverse outcomes. We believe this method can be used to optimize treatment decisions for patients in the intensive care unit," says senior author Aaron Aguirre, MD, Ph.D., an attending cardiologist and critical care specialist at MGH and an assistant professor of Medicine at Harvard Medical School.
Dr. Aguirre's team will conduct additional studies to understand how tissue perfusion pressure varies with different therapies. They also plan to design clinical trials to test whether their new method can help guide clinical care and improve health outcomes in critically ill patients.
More information: Aaron Aguirre et al, Tissue Perfusion Pressure Enables Continuous Hemodynamic Evaluation and Risk Prediction in the Intensive Care Unit, Nature Medicine (2023). DOI: 10.1038/s41591-023-02474-6 www.nature.com/articles/s41591-023-02474-6




















