This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Genetic predisposition linked to whether depression leads to other diseases
Almost one in five Danes experiences depression during their lives. A new study from Aarhus University now shows that the genetic risk of depression can be linked to an increased genetic risk of other psychiatric diagnoses. The study has just been published in Nature Medicine.
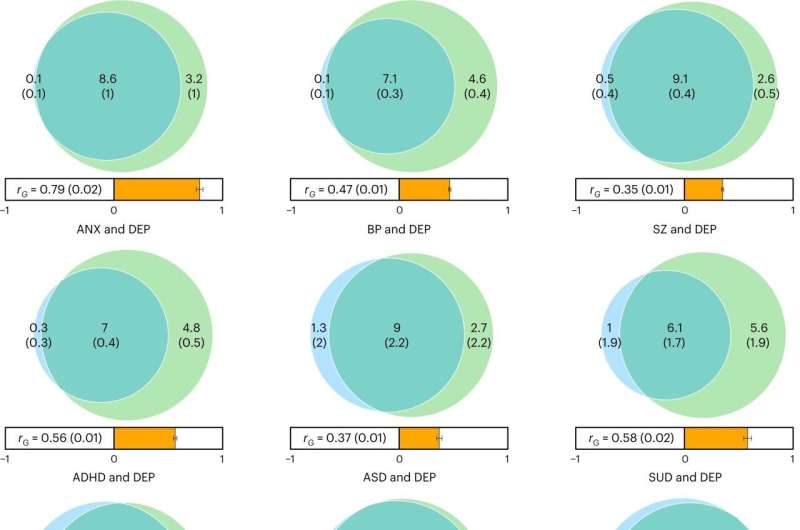
Through a detailed genetic scan, the researchers studied the genome of 1.3 million people, where more than 370,000 of them suffered from depression. This is the largest genetic study of depression to date, and it shows that people with hospital-treated depression often have a higher risk of developing diseases such as substance abuse, bipolar disorder, schizophrenia and anxiety disorders, and that it is possible to predict the risk of developing these psychiatric disorders using genetic analyses.
The study shows for instance that people with hospital-treated depression and a high genetic predisposition to bipolar disorder are 32 times more likely to develop the disease than the rest of the general population.
Similarly, people with hospital-treated depression and a high genetic predisposition to schizophrenia are 14 times more likely to develop schizophrenia compared to the rest of the population.
New prevention and treatment options
The results pave the way for offering high-risk people preventative measures and early treatment in the future, says professor Anders Børglum from the Department of Biomedicine at Aarhus University and iPSYCH (national initiative for integrative psychiatric research), who led the study.
"For example, targeted efforts that offer more frequent monitoring for the development of bipolar disorder, schizophrenia and anxiety among people with depression who have the highest genetic and clinical risk of being diagnosed with one of these disorders. This would enable early diagnosis and treatment, which we know can have beneficial effects."
Likewise, according to Anders Børglum, identifying people with depression and a high genetic risk of developing substance abuse could make the patient and the doctor aware of the issue. Preventative measures could then be initiated to prevent the development of substance abuse.
The study shows that people with hospital-treated depression and a high genetic predisposition to substance abuse have a 21 percent risk of developing a serious substance abuse problem. This is more than five times higher than the group with a low genetic predisposition to substance abuse who have also had a depression. And ten times higher than the general population without hospital-treated depression. This group only has a 2 percent risk of being diagnosed with substance abuse over the same period of time.
Negative effects on an individual's brain function and level of education
In the study, the researchers found many new genetic risk variants and risk genes for depression. These provide new knowledge about the biological disease mechanisms involved and point to new molecular targets for treatment.
"We found a number of biological systems and cell types that are affected by the genetic risk. The effects are seen in virtually all regions of the brain, but not in other organs. And mainly in the brain's nerve cells—neurons," says Thomas Als, former associate professor at the Department of Biomedicine and the first author of the article.
"The genetic risk can affect many different types of neurons. Overall, it can be said that the genetic risk affects the development and communication of brain cells," says Thomas Als.
The study shows that a total of 11,700 genetic risk variants can explain 90 percent of the heritability of depression, making depression one of the most complex and polygenic mental disorders. The majority of the risk genes still need to be identified.
The researchers have discovered that virtually all of the 11,700 genetic risk variants for depression also have an impact on the level of education of the general population. Some risk variants increase the likelihood of completing higher education, while others reduce the likelihood. However, overall, the genetic variants reduce the likelihood of a person completing higher education.
"In line with this, we found that genetic risk of depression is linked to reduced cognitive properties in the population. This particularly affects abstract thinking and mental flexibility, attention and verbal reasoning," explains Anders Børglum.
Depression can be a serious and severely debilitating condition. The results of the study indicate that the seeds of the disease are already being sown in the embryonic stage.
"We found evidence that part of the genetic risk is already influencing brain cells in the embryonic stage, and that depression to some extent is a neuronal developmental disorder," says Anders Børglum:
"This tracks with the fact that we're seeing a significant genetic overlap between depression and, for example, autism and ADHD."
More information: Thomas D. Als et al, Depression pathophysiology, risk prediction of recurrence and comorbid psychiatric disorders using genome-wide analyses, Nature Medicine (2023). DOI: 10.1038/s41591-023-02352-1


















