This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
The landscape of opioid prescribing has changed, but is it for the better?
Globally, opioid prescribing has increased significantly over the past three decades. In 2019, Australia had the eighth highest level of opioid use in the world.
Although opioids play an important role in managing pain, increases in prescription opioid use has led to more opioid related deaths. In the 10 years from 2007 to 2016, opioid-related mortality doubled from 591 to 1119 in Australia, with most deaths attributed to prescription opioids. Prescription opioids are used for medical treatment (e.g., for pain or opioid dependence treatment), and for nonmedical reasons (e.g., for their euphoric effects). Harms can occur with both medical and nonmedical use.
In an attempt to reduce harm from prescription opioids, a number of changes have occurred in Australia.
What changes have occurred?
In June 2020, the government made several changes to the Pharmaceutical Benefits Scheme (PBS) which influenced the way doctors prescribe opioids. This included reducing the pack sizes of opioids (e.g., boxes of 10 tablets instead of 20 tablets) when prescribing opioids for acute pain, and changing the criteria and instructions for doctors prescribing opioids for chronic pain.
In more recent years, prescription monitoring programs have been adopted by all Australian jurisdictions. These programs aim to reduce harm from medicines such as opioids by alerting doctors and pharmacists to patients who may be seeing multiple prescribers, attending multiple pharmacies and those receiving high doses or high-risk drug combinations. While on the face of it, this is a good move, evidence to show the impact of these systems is lacking.
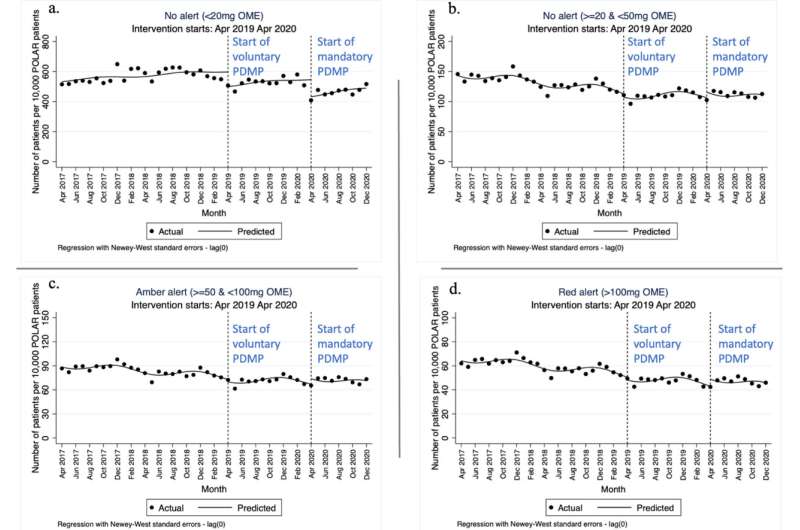
A study published in July in the International Journal of Drug Policy has looked at opioid prescribing in more than 450 Victorian General Practices before and after the introduction of voluntary and mandatory prescription monitoring. No impact on overall prescribing rates of high dose opioids or high-risk combination prescribing was found—which runs counter to the expectations of the program. Some evidence of a "substitution effect" was identified, with increases in prescribing of other medicines such as pregabalin and tricyclic antidepressants (which can bring their own risks and harms) coinciding with the introduction of the program.
Recent changes have also been made to the Opioid Dependence Treatment Program. These changes allow medicines for the treatment of opioid dependence to be subsidized under the PBS, reducing the cost to the individual. Now, more than 50,000 Australians who access opioid dependence treatment will save thousands of dollars, with costs now aligned with other common medicines.
While many health care workers are supportive of the change, others who provide the treatment say the program has been rushed through and it is no longer economically viable for them to provide care. The concern is that this change that was meant to make access easier, may make treatment less available.
What happened in the United States of America (US) with opioid prescribing?
In the U.S., large reductions in opioid prescribing followed the implementation of prescription monitoring systems and the 2016 CDC Clinical Practice Guideline for Prescribing Opioids.
Although this was the intended outcome, well documented adverse effects have been associated with reduced opioid prescribing. These include increased overdose and mental health impacts, particularly when opioids are stopped abruptly or involuntarily, or where people did not receive care for pain or opioid dependence.
A large increase in opioid-related deaths followed shifts from prescription opioid use to unregulated illicit opioid use. This includes deaths from the use of falsified (counterfeit) pharmaceutical pills containing the highly potent synthetic opioids like fentanyl and nitazenes. Concerningly, similar detections have been reported in Australia.
Concerns about initiatives directed at limiting prescription opioid use have now been raised in Australia. Individuals and organizations have highlighted the need to minimize unintended harms and protect access to opioids where they are beneficial for patients.
What is Australia doing differently?
While Australia and the U.S. have both implemented prescription drug-monitoring programs, Australia has taken a health rather than law enforcement approach. Prescriber fear of retribution in the U.S. may have been the cause of the large numbers of patients being cut-off high dose opioids. Although analysis around prescription monitoring implementation in Australia has not found large reductions in high-dose opioid prescribing, recent reports have found people with chronic pain in Australia report some similar difficulties accessing opioids.
In addition to changes by the government, there have been recent initiatives to support doctors and patients to plan to reduce opioid doses together.
In 2023, a guideline was launched in Australia, based on research on the best way to reduce opioid doses. Learning from the harms observed in the U.S., and acknowledging challenges faced by people who rely on opioids for pain management, this guideline has quite a different focus. It specifically recommends that opioids be tapered gradually and that doctors make plans alongside their patients, which consider their goals and preferences. Importantly, the guideline recognizes that stopping opioids is not for everyone.
Time will be needed to assess the impact of these changes, but the hope is that the different approach to implementing these systems in Australia will mean that the dramatic increase in opioid harm seen in the U.S. is not mirrored here.
More information: Suzanne Nielsen et al, Changes in opioid and other analgesic prescribing following voluntary and mandatory prescription drug monitoring program implementation: A time series analysis of early outcomes, International Journal of Drug Policy (2023). DOI: 10.1016/j.drugpo.2023.104053





















