This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Closing in on a cure for common leukemia
A leukemia test can help identify patients who are strong candidates for lifelong treatment free remission (TFR)—meaning they are effectively cured of the disease.
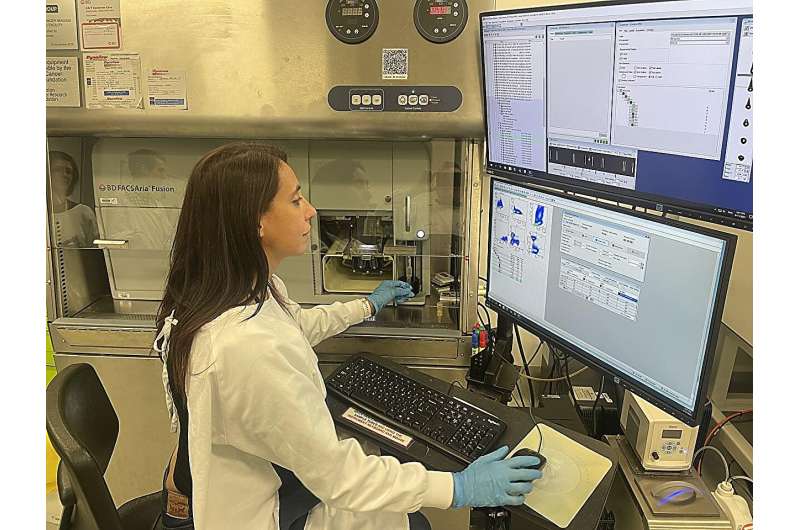
Dr. Ilaria Pagani is first author on the research paper which was published today in the journal Blood. She says the breakthrough in chronic myeloid leukemia (CML) research is the cumulation of six years of investigation.
"With this discovery, we move the conversation for people with CML from one of lifelong disease control to one of cure," she said.
"With the test we have developed, we can predict with a high degree of accuracy who will have an excellent probability of ongoing TFR."
Research into CML has made life-saving discoveries over the past few decades. In the early 1990s, the disease brought an average survival rate of less than five years.
The development of tyrosine kinases inhibitors (TKIs) as a treatment dramatically increased survival rates, but for many patients caused debilitating side effects while losing efficacy over time. Ensuing decades of diligent research saw next-generation TKIs developed to deliver longer-lasting impact and less side effects, but still patients faced lifelong management of the disease.
By 2006, work led by Dr. Pagani's Adelaide-based colleagues A/Prof David Ross and Prof Tim Hughes, in collaboration with international teams, showed that it was possible for patients who had excellent responses to treatment to simply stop taking their medication and remain in remission. For those people who could sustain it, TFR is effectively a cure, but there was still no way to tell who would be successful and who would relapse and need to restart therapy.
Today's findings are significant because they challenge an existing assumption that response to TKI therapy is best assessed by measuring the presence of the leukemia-defining BCR::ABL1 fusion gene in the blood of a CML patient.
"Until now, the assumption was that every blood cell that contained BCR::ABL1 was evidence of persistent disease that could lead to relapse," Dr. Pagani said.
"What we have now shown is that the chances of relapse depend greatly on which type of cell the disease is detected in—if it's in what are known as myeloid cells, then the chances of TFR are sadly pretty low, but if it's in lymphocytes then that has limited impact on relapse likelihood."
This research involved a broad collaboration between Dr. Pagani's SAHMRI-based team, the University of Adelaide, the University of South Australia, Flinders University, SA Health and Perth-based researchers.
The material outcome is a blood test that more accurately determines the best course of treatment, giving TFR candidates greater confidence before ceasing treatment.
"This new lineage-specific BCR::ABL1 test can now be used to determine who can safely stop therapy, who should continue therapy for a longer period, and who needs a different therapy before they could be considered for TFR," Dr. Pagani said.
"Sadly, not everyone will be a candidate for TFR with current approaches, but for those whose chance of relapse is high, we will now have greater information with which to design new therapeutic approaches that can lead to TFR even for these more challenging patients.
"Ultimately, our aim is to design a curative approach for all CML patients so that TFR becomes the mainstream pathway, rather than a pathway followed by a lucky minority."
CML is a relatively rare leukemia in terms of diagnosis, but the success of researchers and clinicians to improve survival rates mean it is an increasingly common for people to be living with the condition.
CML causes the bone marrow to produce too many white blood cells which can adversely affect normal blood cell production. In time, a shortage of blood cells can present as infection, anemia, or unexplained bleeding or bruising. People with CML might also experience discomfort beneath their ribs on the left-hand side of their body due to an enlarged spleen.
More information: Ilaria Stefania Pagani et al, Lineage-specific detection of residual disease predicts relapse in chronic myeloid leukemia patients stopping therapy, Blood (2023). DOI: 10.1182/blood.2023021119


















