This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Researchers build online glaucoma simulator
Researchers at the University of Toronto have built an online simulator that gives an improved visual representation of the deterioration caused by glaucoma.
The simulator, built by Professor Willy Wong and Ph.D. candidate Yan Li of the Faculty of Applied Science & Engineering and their collaborators, depicts the disease from the patient's perspective.
Almost all other representations on the internet are inaccurate, says Wong.
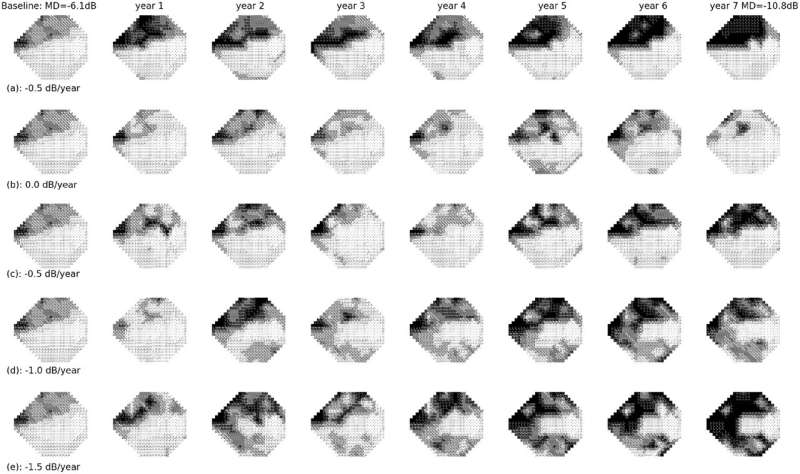
"If you do an internet search for what glaucoma looks like, the images returned are tunnel vision with the periphery blacked out. There's very little truth to this," says Wong of the Edward S. Rogers Sr. department of electrical and computer engineering. "What's really happening is patches of your visual field are losing their spatial integrity—more what you might see when you just wake up, when you're not really focused in."
Wong and Li's online simulator is based on a data-driven model they developed to help quantify glaucoma measurements. Their model, which takes into consideration the physiological mechanism of the eye, was recently published in a paper in the journal Translational Vision Science & Technology.
"We worked closely with glaucoma specialists—two are co-authors on the paper—and they helped us get up to speed with the pathophysiology of the eye," Li says. "Working side by side with them, we got precious first-hand experience about what clinicians need from technology."
Glaucoma tends to affect older individuals and is generally painless. The disease is characterized by elevated pressure in the fluid that fills the eyeball, which then compresses and damages the nerve endings that transmit signals to the brain.
The disease is a leading cause of blindness, but its progression can be greatly slowed with medication and other interventions. To determine when these are needed, doctors routinely perform proactive monitoring, which includes several qualitative tests, such as examining the optic nerve or the retinal layer. These typically employ numbered measurements to be as precise as possible.
"But even with these measurements, the doctors don't always know if it's trending upwards or downwards or staying the same," says Wong.
This is because many of the physiological measurements are inherently noisy. For example, visual field tests rely on the measurement of visual thresholds—that is, the minimal amount of energy required to see—but these thresholds can be unreliable. The noisiness is also compounded by the many years over which the tests are taken and the gaps where appointments are inevitably missed.
Li says that what makes this model unique is the way it combines data from these tests with knowledge about the biology of the eye.
"You have to be mindful of how the nerves go from the eye itself—from the visual field into the optic disc," he says. "If you know the relationship between the two and add that causality to the clinical data, you have a much better prediction tool."
Wong and Li's online simulator allows the user to set the patient's age range and control progression rates from a starting point of mild, moderate or severe. It then simulates the yearly progression of the disease through photos of people, landscapes and city scenes.
"I showed an ophthalmologist our simulator and he said, 'This is exactly what I need,'" says Wong. "Glaucoma is so slow in developing, it's apparently hard to convince patients to take the medication because they don't see or understand the difference."
Li's next step in this project is to combine different testing methodologies for glaucoma to shorten the time required to reliably detect its onset using machine learning (ML) methods. Faster detection will allow for sooner intervention and a better chance at stopping the irreversible loss of vision, he says.
"The development of medicine relies heavily on doctors passing their experience to one another, and ML helps to quickly and efficiently learn and transfer the knowledge from domain experts," he says. "This is a major benefit of the era of big data in health care."
"Combining computing power with deep knowledge of biology, such as Wong and Li have done, is very compelling," says Professor Deepa Kundur, who chair of the electrical and computer engineering department. "The results speak for themselves, and I wouldn't be surprised to see this hybrid model make a difference in other applications."
More information: Yan Li et al, A Data-Driven Model for Simulating Longitudinal Visual Field Tests in Glaucoma, Translational Vision Science & Technology (2023). DOI: 10.1167/tvst.12.6.27


















