This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Dysfunction of mitochondria drives the exhaustion of T cells, study shows
In the immune system's fight against cancer and infections, the T cells often lose their power. The team of Würzburg immunologist Martin Vaeth has found a possible explanation for this phenomenon.
In the immune system, chronic infections and the defense against tumors often lead to the phenomenon of T cell exhaustion: In this process, the T lymphocytes gradually lose their function, which impairs their responses against cancer and infections. The molecular mechanisms that control this loss of function have not been fully unraveled.
This research has now shown that the exhaustion process is significantly influenced by the "powerhouses of the cells," the mitochondria.
When mitochondrial respiration fails, a cascade of reactions is triggered, culminating in the genetic and metabolic reprogramming of T cells, a process that drives their functional exhaustion. But this "burnout" of the T cells can be counteracted—pharmacological or genetic optimization of cellular metabolism increases the longevity and functionality of T cells. This can be achieved, for example, by overexpressing a mitochondrial phosphate transporter that drives the production of the energy-providing molecule adenosine-triphosphate.
These discoveries are reported by a team led by Vaeth at the Institute for Systems Immunology at Julius-Maximilians-Universität (JMU) Würzburg in the journal Nature Communications. "We are optimistic that our findings will contribute to the improvement of cancer immunotherapy," the scientist says.
Possible improvement of CAR-T cell therapy
As an example, CAR-T cell therapy has demonstrated remarkable efficacy in the treatment of leukemia and lymphoma. CAR-T cells are lymphocytes that that have been engineered in the laboratory to fight the respective form of cancer. However, when it comes to solid tumors, CAR-T cells also tend to experience exhaustion, limiting their success in this context.
"Our experiments demonstrate that augmented mitochondrial metabolism also increases the longevity and functionality of virus-specific T cells in chronic infections," says the JMU scientist. It is plausible that this strategy can be also harnessed to enhance T-cell-based immunotherapies for cancer therapy.
The experiments
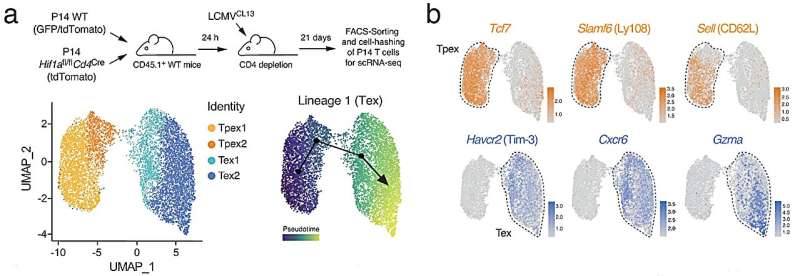
"It was commonly assumed that the observed alterations in the mitochondrial (energy) metabolism were a consequence of T-cell exhaustion," says Vaeth. To demonstrate that mitochondrial dysfunction is the actual cause of T cell exhaustion, his research group developed a new genetic model. It switches off the mitochondrial phosphate transporter (Slc25A3) and paralyses mitochondrial respiration in T cells.
As a result, the T cells are forced to switch to alternative metabolic pathways, mainly aerobic glycolysis, to meet their bioenergetic demand in the form of adenosine triphosphate. However, this metabolic adaptation causes an increased production of reactive oxygen species in the T cells.
Elevated levels of oxygen radicals prevent the degradation of the transcription factor hypoxia-inducible factor 1 alpha (HIF-1α). The accumulation of HIF-1α protein causes a genetic and metabolic reprogramming of the T cells, accelerating their exhaustion.
"This HIF-1α-dependent control of T-cell exhaustion was previously unknown. It represents a critical regulatory circuit between mitochondrial respiration and T cell function, serving as a 'metabolic checkpoint' in the process of T-cell exhaustion," explains Vaeth.
Considering tissue as the environment of T cells
Next, Vaeth's team wants to explore how mitochondrial respiration influences the epigenetic programming of T cells, for example through post-translational modifications of histones, and the interplay of T-cell metabolism with the local tissue microenvironment.
According to Vaeth, this is particularly important because the nutrient supply and oxygen tension in tumors differ considerably from healthy tissue and T cells must actively respond to this challenging environment. New technical developments, such as spatial transcriptome and metabolome analyses, offer exciting new possibilities for investigating these questions systematically and at high resolution in the context of the tissue microenvironment.
More information: Hao Wu et al, Mitochondrial dysfunction promotes the transition of precursor to terminally exhausted T cells through HIF-1α-mediated glycolytic reprogramming, Nature Communications (2023). DOI: 10.1038/s41467-023-42634-3



















