This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Tumor antigens key to improving cancer immunotherapy, study suggests
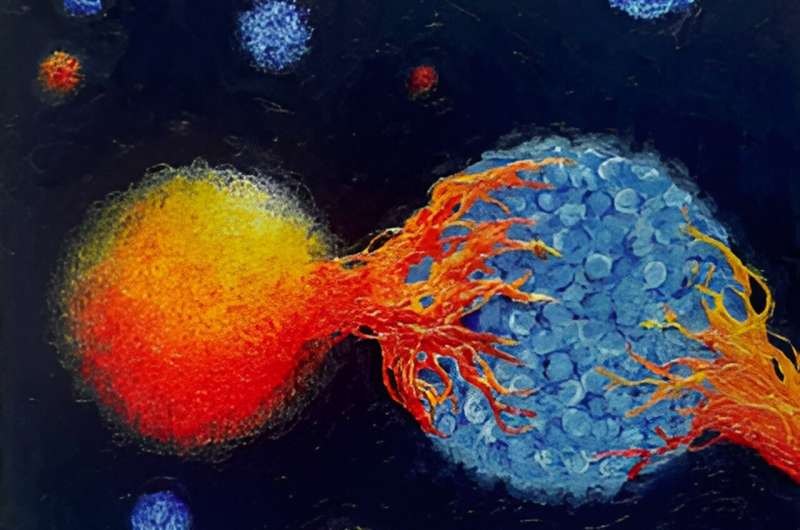
Just as the body's immune system can fight off infection, it can be a powerful weapon against cancer. Harnessing and fine-tuning that weapon, however, will require a better understanding of the complex interactions between immune and tumor cells.
Mary Philip, MD, Ph.D., a cancer specialist at Vanderbilt University Medical Center, has been studying ways to improve the efficacy of cancer immunotherapies such as immune checkpoint blockade (ICB), which removes the natural brakes on proliferation and activation of cytotoxic CD8+ immune T cells.
In her group's latest paper, published in the journal Cancer Immunology Research, Philip and her colleagues report that the type of tumor antigen encountered by the CD8+ cell, and whether that encounter occurs against a backdrop of inflammation, influences how well it will respond to the tumor.
"By understanding how the type of tumor antigen and the tumor context impact CD8+ T cell responses, we can better design immune therapies that attack tumors without also attacking healthy normal tissue in patients," said Philip, assistant professor of Medicine in the Division of Hematology and Oncology and Pathology, Microbiology, and Immunology.
Tumors carry two different kinds of antigens. One type is a mutated, tumor-specific antigen, displayed only by tumors. The other, a self/shared antigen, is also carried by the normal tissue from which the tumors arose.
Immunotherapies such as ICB can cause tumors to shrink by triggering immune responses against either tumor antigen. However, immune responses against self/shared antigens can damage normal tissue. This toxic reaction, known as an immune-related adverse event (irAE), can limit the use of ICB therapies.
"We still do not understand why ICB therapies cause tumor regression in some patients with cancer and irAE in others," Philip said.
Philip and her colleagues previously developed a genetic mouse model in which the mice develop liver tumors as they age in a similar way to humans.
In this study, they took their model one step further by engineering the tumors to express both tumor-specific and self/shared antigens. This allowed the researchers to track immune responses against both types of antigens as tumors develop.
Jess Roetman, Ph.D., who completed her graduate degree in the Vanderbilt Program of Cancer Biology, is first author of the current study, which found significant differences between CD8+T cell responses depending upon which tumor antigen was recognized.
Tumor-specific CD8+T cells, those recognizing tumor-specific antigens, lost function over time, whereas those recognizing self/shared antigens not only lost function but also disappeared rapidly from the liver tumors in which they were being studied.
Interestingly, the team found that these self/shared antigen specific CD8+ T cells persisted long-term in the spleen, and though they expressed surface markers and transcription factors associated with functional memory T cells, remained dysfunctional.
Two other factors may be important in determining how CD8+ T cells respond to tumors.
In 2022, Philip and her colleagues at Memorial Sloan Kettering Cancer Center reported evidence of a "Goldilocks" range for T-cell receptor signal strength, a measure of T-cell affinity for its antigen.
Affinity that is too high leads to a dysfunctional response, whereas affinity that is too low, often the case for self/shared antigens, results in inertness—no response at all.
In addition, T cells responding to self/shared tumor antigens in the presence of immune checkpoint blockade may require "priming" by inflammatory and infection-induced cytokines before they will proliferate, differentiate, and attack tumor cells.
Philip and her team have previously reported that within hours of encountering a tumor, CD8+ T cells became dysfunctional, or "exhausted," and no longer able to mount an attack against it. In comparison, the cells remained functional and battle-ready when confronted by an acute infection.
"Based on our findings, we are now testing strategies in our mouse cancer models to modulate antigen context and affinity to improve anti-tumor T cell responses," she said. "Our goal is to develop new immunotherapies that kill tumor cells without attacking healthy tissue in patients."
More information: Jessica J. Roetman et al, Tumor-Reactive CD8+ T Cells Enter a TCF1+PD-1− Dysfunctional State, Cancer Immunology Research (2023). DOI: 10.1158/2326-6066.CIR-22-0939



















