This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Researchers find promising candidate to treat irreversible lung and eye diseases in extremely premature infants
Novel findings reported in The American Journal of Pathology implicate granulocyte colony-stimulating factor (G-CSF) in both bronchopulmonary dysplasia and retinopathy in premature babies
Advancements in the care of premature babies are leading to improved survival rates. However, the incidence of neonatal diseases with life-long consequences, such as bronchopulmonary dysplasia (BPD) and retinopathy of prematurity (ROP), is increasing. A novel study has implicated granulocyte colony-stimulating factor (G-CSF) in both BPD and ROP, making it a promising therapeutic candidate.
BPD, also called chronic lung disease of immaturity, afflicts approximately one-third of all highly premature infants, causing lifelong lung damage. It occurs in approximately 80% of infants born between 22 and 24 weeks of gestation. There is no effective treatment other than supportive care. BPD often occurs alongside the neonatal eye disease ROP, which impairs vision irreversibly, suggesting a related pathogenesis. However, specific mechanisms of BPD and ROP remain unknown.
Lead investigator Margaret L. Hibbs, Ph.D., Leukocyte Signalling Laboratory, Department of Immunology, Central Clinical School, Monash University, explains, "Our laboratory focuses on inflammation and its underlying mechanisms, and we have been studying myeloid colony-stimulating factors for many years. Previous work by us reported that G-CSF was pathogenic in chronic obstructive pulmonary disease (COPD), and this has now been shown by others to occur in asthma."
"Given the links between early life lung disease and COPD, it seemed reasonable to hypothesize that G-CSF may also be implicated in the neonatal lung disease BPD."
Investigators used a neonatal mouse model of coincident BPD and retinopathy to screen for candidate mediators. Equal numbers of male or female mice were assigned randomly to normoxia (21% oxygen) or hyperoxia (75% oxygen) and were exposed within 12 hours of birth.
The study revealed that G-CSF was significantly induced in mouse lung wash fluid and plasma in response to hyperoxia. This was validated in human disease as preterm infants with more severe BPD had increased plasma G-CSF.
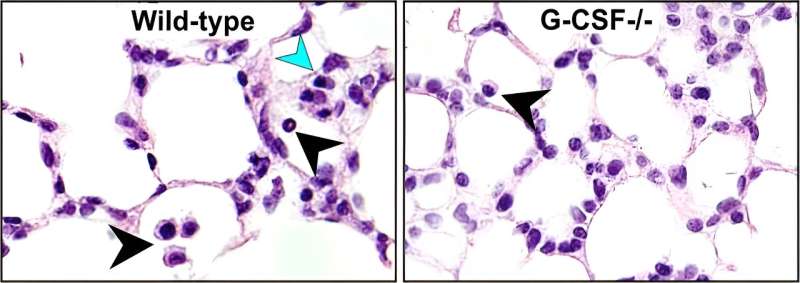
Neonatal mice deficient in G-CSF exhibited significantly reduced alveolar damage and, correspondingly, showed minimal impairment of lung function following exposure to hyperoxia. This was associated with an ameliorated oxidative stress response, reduced lung epithelial cell proliferation, decreased migration of myeloid cells from the periphery into the lungs, and diminished myeloid cell activation. Deficiency of G-CSF also protected against retinopathy, suggesting wide-ranging protection.
Professor Hibbs notes, "Inflammation is highly implicated in the pathogenesis of BPD, so we speculated that G-CSF–dependent inflammation might be involved in this lung disease, but the surprise was that deficiency of G-CSF also protected against retinopathy. While more needs to be done to expand these findings, recent studies implicate neutrophils in ocular diseases such as ROP and diabetic retinopathy, and G-CSF is the major regulator of neutrophil development survival and activation."
Co-investigator Evelyn Tsantikos, Ph.D., Department of Immunology, Central Clinical School, Monash University, comments, "These studies produced some surprises, including the unexpected protection that G-CSF deficiency afforded to the endothelial compartment. While this may relate to the reduced oxidative burden, G-CSF receptors have been shown to be expressed on endothelial cells, so we are keen to investigate this finding further."
First author Lakshanie C. Wickramasinghe, Ph.D., Department of Immunology, Central Clinical School, Monash University, adds, "These studies highlight the value of collaborative research—we could not have achieved the best research outcomes without involving clinical collaborators, Professor Atul Malhotra, who provided a first-hand look into the respiratory interventions provided in the neonatal intensive care unit; and Professor Anne Hilgendorff and Dr. Alida Kindt, who performed translational studies in BPD patients demonstrating significantly elevated levels of G-CSF in infants with more severe BPD."
Professor Hibbs concludes, "Our studies identify a new mechanism in BPD that is therapeutically tractable and may help rescue the lungs and sight of infants from life-long damage. Neonatal lung and eye diseases are currently managed and treated as independent conditions. However, our findings suggest that G-CSF is a pathological mechanism common to both, which may advance a new therapeutic strategy to improve the care and long-term outcomes of these vulnerable premature infants."
More information: Lakshanie C. Wickramasinghe et al, Granulocyte Colony-Stimulating Factor is a Determinant of Severe Bronchopulmonary Dysplasia and Coincident Retinopathy, The American Journal of Pathology (2023). DOI: 10.1016/j.ajpath.2023.07.006


















